We are glad to publish the contribution of Dr Fabrizio Gervasoni and Dr Arnaldo Andreoli, Rehabilitation Unit, “Luigi Sacco” Hospital, ASST Fatebenefratelli Sacco – Milan, Italy.
My view, you know, is that the ultimate destination of all nursing is the nursing of the sick in their own homes…
With these words, Florence Nightingale, the inspirer of modern nursing care, on Easter Sunday 1867 foreshadowed a health system capable of treating patients in their homes. Home care, whether nursing or physiotherapy, already represented a valuable care opportunity for patients who could not be transported or, for some reason, were unable to reach hospital facilities for outpatient treatment. The COVID-19 pandemic, however, has required a rapid acceleration of many processes, in particular technological innovation, and in a very short time many experiences in Telemedicine and Telerehabilitation in support of patients treated for SARS-CoV-2 infection, but also of all patients unable to access hospital care due to the restrictive lockdown measures.
The rehabilitation needs of patients with a post-COVID syndrome
In the first weeks of the SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) pandemic emergency, all the dramatic aspects of Coronavirus Disease 19 (COVID-19) with increasing respiratory problems, up to the need for respiratory support in the ICU, have been extensively described and deepened.
Physiatrists and physiotherapists of the Specialized Rehabilitation Unit of the “Luigi Sacco” Hospital in Milan, Fatebenefratelli Sacco Local Health Authority, were very early involved in the rehabilitation of patients diagnosed with COVID-19 [1].

In the requests received from the numerous and different wards, however, only 12% asked for an evaluation to set up a rehabilitation treatment of respiratory rehabilitation. In comparison, 26% of the requests were motivated by the bedding syndrome resulting from the extended stay of patients in intensive care. However, the most significant element is that more than 24% of the requests expressed rehabilitation needs not limited to respiratory problems, but showed neurological or neuromotor deficits [2]. Over the emergency weeks, therefore, it was more and more evident how COVID-19 was not only a respiratory pathology but, on the contrary, it involved the whole organism, configuring a real “syndrome” with numerous and heterogeneous clinical presentations, from stroke to Critical Illness Myopathy and Neuropathy (CRIMYNE), from sensory-motor polyneuropathy to the suffering of single peripheral nerves from extrinsic compression, from the allurement syndrome, up to widespread myalgia.
The multiple rehabilitation needs persisting after the resolution of the acute phase of COVID-19 were increasingly evident. The complexity and heterogeneity of clinical presentations, therefore, has imposed the need to prepare highly individualized physiatric evaluations with the consequent setting of Individual Rehabilitation Projects (PRI) customized for each patient.
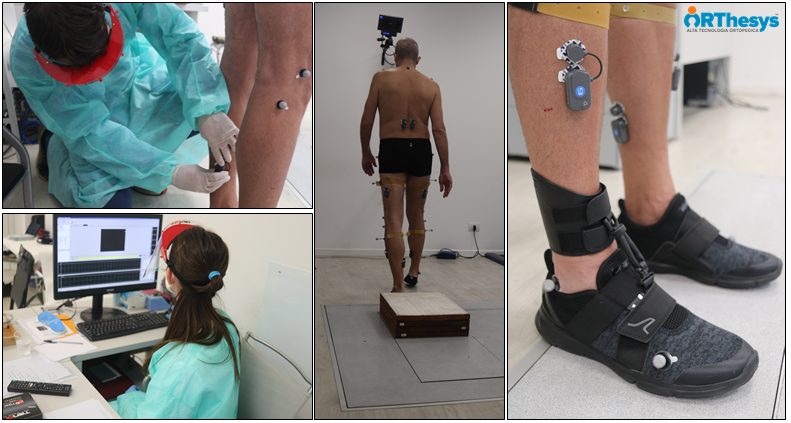
High technology equipment is a crucial opportunity for this purpose. For this reason, the team of the Hospital “Luigi Sacco” has started a collaboration with Prof. Andrea Aliverti and Eng. Antonella Lo Mauro of the Department of Electronics, Bioengineering Information of Politecnico di Milano for the execution of optoelectronic plethysmography for the study of respiratory mechanics and with the Gait Lab of Orthesys for the execution of movement analysis of patients with the post-COVID syndrome. In this way, thanks to the support of sophisticated technological systems, it was possible to identify the respiratory and neuromotor consequences of COVID-19.
Narrative Medicine and Personal Protective Equipment (DPI)
The rehabilitation process of patients with COVID-19, however, has started since their stay in the Intensive Care Unit.
Doctors, nurses and physiotherapists, in the emergency period, had to experiment and discover new methods and languages of care, experiencing daily the need to take charge of patients in isolation. Every clinical evaluation was conditioned by therapeutic measures (such as respiratory helmets) and Individual Protection Devices (PPI): masks that concealed the smile, made it difficult to breathe and marked the face, visors or glasses, double gloves and water-repellent gowns. The encounter with health care providers, however, was in many cases the only way for patients to interface with the world, and their gaze was the most eloquent glimpse to seek an emotion or hope of cure [3].
Healthcare professionals, therefore, had to discover, invent and develop new languages of care and new communication strategies: to reassure the patient and share with him/her the care path, to inform family members or to put them in contact with patients thanks to tablets and smartphones. Contact and communication times extremely condensed and, often, conditioned by the interposition of DPI or technological communication devices, have forced clinicians to “reinvent themselves”, developing new strategies and discovering new solutions for taking charge of patients.
Is it possible to remain “klinikós”, even “from a distance”?
Many people, however, have stayed at home because of the restrictions imposed by the lockdown and have not had the opportunity to access hospital care; for example for the treatment and care of chronic diseases, neurological problems or rare diseases. Telemedicine has, therefore, become an essential tool for the monitoring and sometimes rehabilitation of these patients.
However, the very essence of “clinical” is intrinsic in the proximity of the doctor to the patient’s “bed” (i.e. klínē “bed”), while Telemedicine is, by definition, “from afar” (tele- “far away”). In order to bring these two (apparently irreconcilable) realities closer together, it was necessary to identify appropriate technological tools, checklists for the proper conduct of remote examinations (from the collection of informed consent to the issuance of the report), new clinical semiotics and new languages for the path of patient care.
Telemedicine and COVID-19
Televisit is “a health act in which the doctor interacts remotely with the patient “[4] and can be an opportunity to continue monitoring and rehabilitative treatment of patients with respiratory or neuromotor problems arising as a result of COVID-19.
At the “Luigi Sacco” Hospital in Milan, a Telemedicine and Teleriabilitation service is being activated for patients with the post-COVID syndrome, thanks to the installation of a control station (Khymeia TeleCockpit) for monitoring the rehabilitation exercises performed at home. The patients, from their homes, will be able to perform physiotherapy sessions through a case with a tablet, sensorized devices for the study of movement and a spirometer for respiratory rehabilitation (i.e. VRRS HomeKit).
The perception of the patient: is care real or virtual?
Florence Nightingale, in 1867, concluded by saying:
But it is no use to talk about the year 2000.
Only today, in 2020, that model begins to materialize, thanks to the new high-tech tools that allow doctors, nurses and physiotherapists to “approach”, albeit telematically, patients and their home for Telemedicine, Telemonitoring and Teleriabilitation. Now it is time to study new languages and new ways of conducting the conversation with the patient so that not a single moment of the precious time of care deriving from the relationship between doctors and patients is lost. Good practices, communication strategies and empathy [5] that will become increasingly essential for clinicians who will be called to treat patients in Telemedicine must be implemented. In order for the patient to perceive that the care shared with the clinician is “real”, even though the visit was “virtual”.
Bibliography
Cortelezzi A, Tribocco S, Zanoni MR, Villa MG, Andreoli A. Prerequisites for a rehabilitation intervention protocol in patients with COVID-19.Medici Oggi. April 2020. (Article in Italian)
Pagani R. Neurological implications of new Corona-virus SARS-CoV-2 infection. Medici Oggi. March 2020. (Article in Italian)
Pagani R. Emotions at the time of COVID-19. Medici Oggi. June 2020. (Article in Italian)
Italian Ministry of Health. Telemedicine – National Guidelines.
Cheshire WP, Barrett KM, Eidelman BH et al. Patient perception of physician empathy in stroke telemedicine. Journal of Telemedicine and Telecare. 2020. Jan 27;1357633X19899237. doi: 10.1177/1357633X19899237.
