For decades we have been talking about the quality of life of patients and families. There are indeed many researches that investigate this aspect with the aim of directing the experimental research and raising awareness among stakeholders to many problems that patients face because of their illness. Less frequently, unfortunately, we use to focus our attention on the quality of life of care professionals who revolve around it. Actually, this is an interesting topic to investigate since many often in Italy and around the world healthcare structures are disorganized, with an excessive workload in many professional realities, and protocols too often focused on efficiency and not on effectiveness, leading to a reduction in the quality of working life. Among the most often suffering helping professions, there are numerous and different professional figures not only at the health level. Researches show that a growing number of lawyers, for example, since they often work closely to victims of psychological, moral and physical traumas, are four times more likely to suffer from depression than the rest of the population and have a higher suicide rate and substance abuse inclination.
However, the area in which an excessive negative imbalance in the quality of professional life is still prominent remains in the health sector. There is evidence that negative feeling affects the sector at 360 degrees, spreading not only among doctors, as some might think, but on all those involved in the care team. In a recent study, for example, more than 25% of volunteer ambulance staff suffer from a series of severe symptoms, classified psychologically as post-traumatic stress. Another research on this topic attests that this same psychological syndrome is highlighted in 34% of the nurses interviewed (Beck 2011). In addition, even among mental health professionals, a U.S. study shows that 72% reported anxiety, 62% felt more distrustful of the world around them and 42% reported feeling increasingly vulnerable after treating the victims of Hurricane Katrina that strucks the United States a few years ago (Hooper 2010; Culver-McKinney-Paradise 2011).
Moreover, care fatigue not only affects professional care but often involves also who care for a sick family member at home, a caregiver, as attested by research on primary home care providers to terminally ill patients: the high risk of developing the same symptoms of excessive care fatigue as health professionals are actually there.
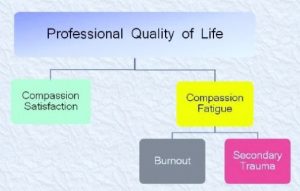
Compassion fatigue is a condition characterized by a gradual decreasing of the desire to care, of the sense of compassion toward patients. The first study on this psychic condition has in fact defined compassion fatigue as a real syndrome, common among professionals who work closely with victims of disasters, traumas or diseases, as the health sector is Characteristic of this syndrome are the acute and sudden appearance, which can be triggered even by a single experience perceived as particularly critical by the person who is affected to. Compassion fatigue was initially studied in the field of traumatology, where it was also called “cost of care” or “the emotional price to pay” for those who care for others. Other non-professional helper syndromes may also be considered as particular compassion fatigue forms, such as the family rape crisis and the “proximity” effects on female partners of war veterans extensively studied in past decades (Day-Anderson 2011-09-08; Figley 1982-1983; McCan-Pearlman 1990-01-01; Remer-Elliot 1988; Erickson 1989; Verbosky-Ryan 1988). Fortunately, the fatigue associated with help has not only negative effects but also a pars costruens, located at the antipodes along this spectrum of the level of job satisfaction, called compassion satisfaction. It is curious to observe how often the same motivational factors that can produce satisfaction in a health professional (and not), in terms of commitment and success or gratitude on the part of their assisted persons, can suddenly turn into the source of discomfort.
Fatigue can manifest itself in different forms, feelings and behaviors, such as episodes of anguish for the consequences on the person assisted, a decreased pleasure and satisfaction felt for their profession, constant stress and anxiety for the accumulation of work and commitment that is now perceived as unsustainable, insomnia or nightmares, and a pervasive negative attitude that can lead to feelings of nervousness and irritation towards the people around us, contributing to isolation and emotional closure. The incidence of this syndrome within the healthcare professions can range from 16% to 85% of the population, depending on the specialist sector but also on the complex and the reality in which they work. In a 2009 study indeed, involving nurses from different departments, about 85% of first aid nurses criteria show symptoms of compassion fatigue (Hooper 2010).
Signs of this condition may also result in Secondary Traumatic Stress (STS) or vicarious trauma. The name comes from the fact that these are emotional wounds resulting from the mere knowledge of traumatic events experienced by others. This condition of strong emotional burden and perceived commitment to care arise in this case from a trauma suffered by another person as a result of the attempt to support this person. STS often manifests itself with intrusive thoughts and loss of perspective on dangers and benefits, unbalancing the perceived focus on dangers. This involves the tendency to avoid any situation that may remind or put in a position to retrace with the mind that traumatic event because it is too painful to endure at a psychological level. Finally, for those who suffer from this form of trauma, the emotional weight of the assistance is particularly unbearable for the person with STS, on the verge of collapsing. Trauma is difficult to talk about, and the challenges of medicine and narrative health care are precisely that of revealing the deep part through the cathartic process of words.
Burnout is another form of compassion fatigue (Beck 2011; Ricard 2015), one of the most serious and drastic consequences of the poor quality of professional life in the helping professions, and involves a total loss of interest in the people to whom the professional should turn their attention and care. In particular, it has been shown that the person in this state constantly experiences an emotional breakdown, tends to implement a depersonalization of the person to be treated, experiencing a reduced personal achievement, frustration and lack of gratification. Maslach, Schaufeli and Leiter (2001) underline that the component of emotional exhaustion emerges as a turning point in the appearance of burn out, resulting from an inner conflict between the request to inhibit their emotions of anger, frustration, and fatigue in the workplace and that of showing empathy in relation to the fact of playing a role of help. Unlike compassion fatigue, burnout is more often related to repeated mismanagement and disorganization of the facilities and institutions where it is performed, rather than to exposure to specific problems of patients such as trauma. It is therefore particularly interesting to point out that often the excessive bureaucracy and the lack of health personnel, affects not only the professional but also the quality of relationship and care with the patient, thus compromising the entire care system. Moreover, this difference with compassionate fatigue also means that Burnout can affect professionals in any professional field, where repetition is obsessive, and it is also to do with the alienation of the type of work, while compassion fatigue is particularly characteristic of the helping professions, which operate in close contact with people who have experienced traumatic events. A further discriminating factor between the two statuses, although overlapping in many respects, is the onset of obvious signs of suffering: compassion fatigue is a feeling that springs immediately and sharply, while burnout is a more progressive and gradual process.
For these reasons, it is clear that the burn out status is an important issue to prevent, monitor, and fight since it affects not only the professional lives but also the entire system globally, the professional relationships, the private and public lives of any kind of workers. With this aim, there are in literature many interesting tools to improve the awareness of professions of help on their level of working satisfaction, on the perceived level of fatigue in providing the care. As we could see from the diagram here reported, an unstable balance between the working satisfaction and the compassion fatigue exists: higher the gratification felt, higher the fatigue to obtain it. A negative disequilibrium of the professional quality of life can, however, increase the risk of STS and burn out.
One of these tools: the Professional Quality of Life Scale (PROQOL) is a validated test, self-submitted, designed by Dr. Figley, one of the most expert in the compassion fatigue field. This test has the aim of evaluating the risk of an excessive relational involvement with the patient, and at the same time, estimating the perceived satisfaction. The test is composed by different items that analyse their personal condition, the identification with their own job, their relation with the working environment and colleagues, and gives a measure of the personal level of the satisfaction, the general risk of burn out, the possibility to feel compassion fatigue, and of the consequences of them as described before. A further method, that was shown effective in self-diagnosed emotional suffering in their work activities, is the narrative. From decennials, reflective writing is diffusely recognized and applied in the field of anti-depressive therapies, of anxiety syndromes, phobias, and mental illness. Not only the patients’ narratives could be analyzed by carers in order to highlight their suffering and illness signs, but also the physicians themselves could notice that something is getting wrong in their own private and professional lives through the narrative (John Launer, 1999; Maria Giulia Marini 2015). Numerous are ISTUD project focused on professional caregivers, and where communicative and educational difficulties in the field of terminal illnesses are largely there (ANALISI DEL CLIMA DI LAVORO NEI CENTRI DI CURE PALLIATIVE – 2006; V.E.D.U.T.A. – 2012), projects able to give voices to common issues of professionals in the management of complex diseases as COPD and severe asthma (Le parole del Respiro 2015; Le parole del Respiro 2016; SOUND 2017). Recently, the Healthcare Area of ISTUD Foundation is working on a real listening work to the voices of neurologists involved in the care of Multiple Sclerosis, in order to evaluate the actual risk of burn out among them (SMART – 2018).
So, what can we do in order to prevent and manage the risk of an excess in compassion fatigue, STS, or burn out? First of all, we have to take care of ourselves: we have to recognize the signs of risk and try a support to prevent or fight problems that lead to fatigue and suffering. Maybe, it could be enough for us, (and it not so easy…) learning how to take patients’ negative emotions, like anxiety and anguish, separately from our professional satisfaction. Further, it could be helpful trying to the deep understanding of our real cut off of stress, leading to increasing information on our susceptibility. Surely, a fair working environment could be helpful to professionals, but too much often their local situations are so complex that changing them could appear out of our possibility; further, high level of stress and burn out could often lead to avoidance, or not to be able to ask for a help and to trust in people. However, the supervision of our work, the teamwork, the relationship with other staff members might contribute to bypass this issue (Dyregrov et al 1996, Lyon 1993). From literature, many studies cited several strategies to help in decreasing the risk: better-organized interviews, if possible, with traumatic patients in order to guarantee them our total attention, but having also the time and the space to restore us psychologically (Trippany et al 2003); learning to balance the working activities, hobbies, and sleeping, to maintain our net of friendly and familial relations, and to improve our coping strategies against the stress condition. Once again, Narrative Medicine could act supporting the professionals through the use in the clinical practice of the parallel chart tool. Further, it could be useful if the Institutions will guarantee a psychotherapeutic service also for professionals, as they did for patients.
Silvia Napolitano, researcher at ISTUD Foundation
Matteo Nunner, collaborator at ISTUD Foundation
