Paola Arcadi is Director of Education of the Bachelor of Science in Nursing at the University of Milan – ASST Melegnano e della Martesana, and President of the Academy of Nursing Sciences (ASI). Always attentive to the human dimension of care, she enriched her path with specific training at ISTUD’s Master in Applied Narrative Medicine, of which she is now also a faculty member. Her practice also reflects an integrated vision of care, in which clinical knowledge and storytelling are intertwined in the awareness that caring also means understanding life stories. Narrative nursing – based on listening, understanding and restitution of experiences – is for her an educational tool, but also an ethical and relational key to rethinking the role of the nurse in the complexity of the contemporary context.
- Paola, your academic and professional career is deeply intertwined with Narrative Medicine. Can you tell us how this interest was born and how it has evolved over time, also in relation to the nursing profession?
My interest in Narrative Medicine did not originate from a theoretical intuition or academic reading, but from a deeply human and professional need for meaning. I have always felt that care, the real care, only happens in the relationship: in that encounter between two stories – mine and that of the person cared for – that intertwine, question and transform each other. It is there that I recognised my nursing identity, which cannot be separated from a relational, reflective and situated vision of the practice of care.
I came across Narrative Medicine at a time when people were beginning to talk, even in Italy, about the urgency of rehumanising care, of restoring centrality to the person in an increasingly technocratic and fragmented system. At first it was like giving a name to something I had always experienced, but which did not yet have a systematic language. It was then through teaching and training, especially in university contexts and in the experiential workshops I helped to build, that I realised how much this approach could become method, knowledge, transmissible competence.
Over time, my view has been enriched by the contributions of the Medical Humanities, phenomenology, narrative pedagogy, but also – and perhaps above all – by the stories heard in hospital corridors, in patients’ rooms, in the stories of students in training. Narrative Medicine, for me, has become a posture, as Paolo Trenta reminds us, even before being a methodology. It is the way I choose to inhabit care, recognising its complexity and cultivating its beauty. This is why I am talking about it today not only as a scholar, but as a witness to a journey that continues to question and transform me.
- In your role as a trainer, you direct your attention to approaches that integrate clinical and humanistic skills. Why do you believe that storytelling should be an integral part of nursing education today?
Because training a nurse today means much more than passing on technical content and scientific updates. It means accompanying a person on a path of transformation, in which one learns not only how to “do”, but above all how to “stay”, how to consciously and responsibly inhabit the relationship with the other, who is often fragile, vulnerable, frightened. Storytelling is the tool par excellence that enables this type of transformative learning.
I teach in a degree course where relational workshops occupy a fundamental space in the curriculum. And not by chance: something radically different happens there than in frontal lectures. Through narration – oral, written, visual – the student gets involved, brings his or her own story, reflects on what he or she has experienced in the workshops, tries to give shape and meaning to often confusing or emotionally intense events. It is in that process of ‘shaping one’s own experience’ that professional awareness is born. It is there that one begins to realise what it means to “be a nurse”, far beyond knowing how to make a dressing or manage a therapy.
Storytelling allows us to hold technical expertise and human depth together. It helps us not to lose sight of the person inside the medical file, not to reduce the patient to a bed number or a diagnosis. It is also an epistemological tool: it teaches us to consider knowledge not only as something to be acquired, but as something to be built together, in relationship. Every story of illness is also a story of possible cure, and every health professional should be able to read it, interpret it, make it his own without betraying its meaning.
This is why I believe that storytelling is not an “extra” in nursing education, but a structural element. At a time when medicine is in danger of becoming increasingly performative, specialised, automated, narration gives us back the complexity of the human and is a competence that is learnt through continuous practice.
- In the academic context, then, how can Narrative Medicine training be made systematic and fertile? What teaching strategies and tools do you use to stimulate this kind of sensitivity and awareness in students?
Making Narrative Medicine training fertile means, first, restoring epistemological dignity to it within the curriculum: not relegating it to sporadic or optional initiatives, but recognising it as a structured, continuous, intentional pedagogical device.
In our Degree Course in Nursing, we have worked a great deal in this direction, building over time a three-year course articulated in relational workshops that are interwoven with moments of practical training. The guiding idea is that storytelling is not just a tool for ‘talking about emotions’, but a training practice capable of transforming lived experience into professional learning.
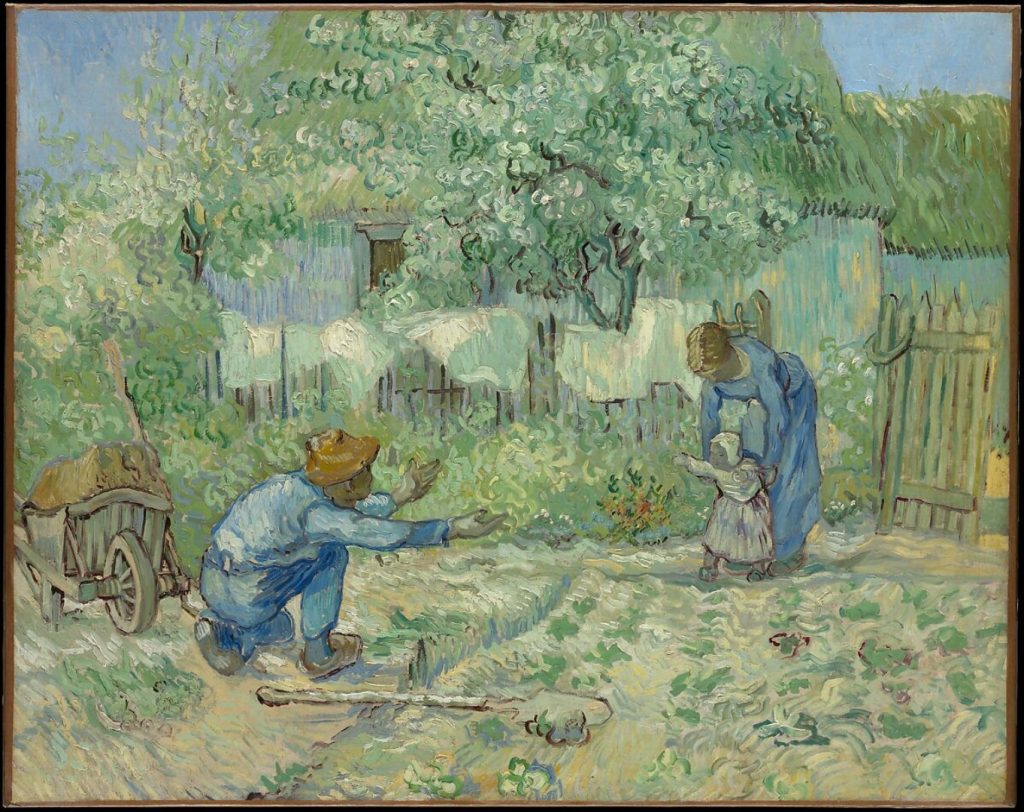
The tools we use are many: autobiographical writing, micro-narratives of clinical situations, close reading of literary texts and images, watching films and documentaries, shared reading of poetic or artistic works. Each activity is designed to foster a profound, often non-linear, but always generative reflective process.
For example, proposing that students recount an episode of their training that touched them, and then read it in the group, means offering them a protected space where vulnerability can be welcomed and listened to. In those moments, something special often happens: the group comes together, a form of collective learning is activated that is not only cognitive but also relational and identity based.
Another example is the work on art: starting from a painting – such as Van Gogh’s ‘The First Steps’ – to reflect on what it means to care, on first times, on uncertainties. This kind of device acts in depth, stimulates resonance, opens spaces of meaning.
But what makes narrative training truly systematic is the consistency of the project over time, its rootedness in the training culture of the course, the competence of the tutors who accompany the process. Narrative, to be educational, needs care.
- What, in your experience, is the response of students to this type of training? What strikes them the most? And how, in your opinion, can storytelling affect their personal and professional development?
Students react with surprise, often with emotion, always with depth. They are not used to being listened to in their innermost dimension. University education – unfortunately – often tends to be performance, evaluation, visible competence oriented. Narrative workshops, on the other hand, offer a space where what counts is not ‘doing well’ but ‘being authentic’.
What is most striking is the possibility of making sense of experiences that would otherwise remain confused, sometimes painful, unprocessed. When a student writes: “I thought I was not good enough, then I told that story and realised that I was not alone, that others had felt that way too”, a change happens. Not only does he feel less lonely, but he starts to see that experience as part of his own growth process.
Storytelling affects professional development because it promotes awareness: of one’s way of being in the relationship, of the emotions that emerge, of the responses that are activated. But it also has an impact on a personal level: it helps to develop empathy, tolerance of ambiguity, and the ability to listen deeply. It teaches that each person carries a story and that the carer’s task is not to judge them, but to welcome them.
In the end, I believe that what most marks the students is the discovery that caring is a profoundly human act, and that their humanity – if cultivated, listened to, educated – is their first and most powerful professional tool.
- In the book “I gatti della signora Augusta e altre storie slow di cura sobria e rispettosa”, of which you are co-author, there is a strong tension between caring, slow time and deep listening. Do you think there is a natural link between narrative nursing and the Slow Medicine philosophy?
Yes, I believe there is a deep and natural link, not only theoretical but experiential, between narrative nursing and Slow Medicine. Both start from the same conviction: care is not measured in technical acts but in the quality of presence. And this quality needs time. Not of chronological quantity, but of Kairòs: that auspicious time that allows for authentic encounter.
In the book I gatti della signora Augusta (Mrs Augusta’s cats), the stories collected are not simply ‘nice’ tales or examples of good practice: they are spaces of resistance against the standardisation of care, against the risk of transforming the act of caring into an impersonal routine. They are stories that demand time and listening.
Narrative Nursing and Slow Medicine also share a common ground of sobriety, respect and justice: three words that are not slogans, but ethical coordinates. Indeed, Giorgio Bert, founder of Slow Medicine and a great teacher of mine, taught us that narrative is not a luxury of care, but a condition of its possibility: because you cannot respect what you do not know, and you cannot truly know if you do not listen to the experience of the other. Not the disease, but his illness, that is, the lived and subjective experience of the disease.
Sobriety requires discernment: it is the ability to choose less when it is more appropriate, to give up what is superfluous or invasive in order to make room for what is essential. But to know what is essential for that person, you need to listen to them. It is necessary to know who she is, what she fears, what she wants, how she imagines her life with – or in spite of – illness.
Respect, likewise, cannot be generic. It is not an abstract attitude, but a concrete practice born of encounter. How can we respect someone if we have never really met them? If we have not made space for their voice, their narrative?
And justice, finally, is not only distributive equity. It is also the relational justice that is built when each person feels seen, recognised, considered worthy of time, attention, speech. Narration is an instrument of justice, because it gives voice to those who often have none, and because it restores to care its two-way dimension.
- Looking to the future, what vision do you have for the role of storytelling in nursing education? Can it represent a stable paradigm, or does it still remain ‘frontier’ territory?
We are still, to some extent, in frontier territory. But a frontier that is alive and on the move. In recent years I have seen a new attention growing towards narrative knowledge, especially in the most innovative educational and training contexts. There is a generation of teachers, tutors, researchers who are seriously investing in Narrative Medicine as a pedagogical, clinical and scientific approach.
My vision is of a nursing that not only recognises but structurally enhances the role of narrative. That integrates narrative devices into the curriculum as stable and transversal elements. Which trains teachers in narrative facilitation, and creates spaces where practitioners too can narrate, rework, find meaning.
Because storytelling is not only a tool to better understand the patient, it is also a tool to take care of ourselves. In a time when the nursing profession is exposed to very strong emotional burdens, the ability to narrate – and to listen – becomes a practice of resilience, of awareness, of safeguarding meaning.
I believe that in the coming years we will see an increasing integration of Evidence-Based Practice and Narrative-Based Practice. And not as a dichotomy, but as an alliance. Because, as Sackett says, evidence only makes sense if it is integrated with patient values. And values are gathered by listening to stories.
- Finally, if you had to express in a few words the meaning of narrative nursing in the education of the new generations, what would be the most urgent message to convey today?
I would say: “Take care of your humanity, because it is the first tool of your professionalism.”
Narrative nursing is not just a technique, but as I said before, a posture. A way of being in the world, and in the encounter with the other. It is what allows us not to become automatic performers, but conscious, reflective, empathic professionals.
To the new generations I often say: do not be afraid of complexity, nor of your vulnerability. They are part of your strength. Learn to listen before you act. Do not be in a hurry to ‘do well’: have the desire to ‘be present’. And never stop telling, for it is in the stories – yours and others’ – that caring takes shape, and that your being a nurse is rooted, strengthened, renewed.
