Psychiatry is defined as: “the field of medicine that has as its object the clinical study and treatment of mental disorders and pathological behavior, distinguished by origin, quality, extent and duration of manifestations” (Encyclopedia Treccani). Among the medical disciplines, psychiatry is historically one of the youngest and, studying the mind as “the part of a person that makes it possible for him or her to think, feel emotions, and understand things” (Cambridge dictionary), has found itself studying an entity with uncertain boundaries with different approaches and methodologies on which finally prevailed the descriptive model of statistical aggregation of symptoms of the American Psychiatric Association (APA) with which the Diagnostic and Statistical Manual of Mental Disorders (DSM) classifies mental disorders. However, by 2013, arriving at the 5th edition of the manual, the neo-positivist model adopted bumped up against the nature of a very different reality that led the authors to admit, “The historic aspiration to achieve diagnostic homogeneity through progressive subtyping of categories within disorders no longer makes sense; like most common human ills, mental disorders are heterogeneous on many levels, ranging from genetic risk factors to symptoms” (APA 2013).
Subtyping is a process analogous to that of Democritus’ atomism, and, moving from him, we have come to discover that atoms are composed of particles, but, having come to this nature of things, the atom-vacuum bipartition is transformed into the complex nature of Heinsenberg’s uncertainty principle, in which, the mind of the observer becomes an integral part of the experimental field, and consequently, a participant.
Particle position, momentum and participating mind, with their (at least) three variables, compose the complex paradigm from which to move to epistemologically approach that dynamic form of understanding, thought and feelings that we call mind. Insisting on reductionism, linear dichotomy, mind-body or biological-psychological dualism means mistaking: “an abstraction or model for the actual reality it represents” (Hustvedt 2016), and from this limitation onwards debasing science into scientism.
Fortunately, the DSM 5, with intellectual honesty, opens to rethinking and, “Willingness to rethink does not mean an inability to discriminate. It does not mean infinite tolerance for crass stupidity, crude thinking, or ideology and prejudice posing as science. (…) It means adopting multiple perspectives because each has something to tell you and none, by itself, can contain the truth of things” (Hustvedt 2016).
In this perspective I would like to propose a small contribution through a qualitative-quantitative study carried out on a population of psychiatric patients during the pandemic by integrating Narrative Medicine to standardized assessment measures. During the second lockdown, from March to June 2021 in a residential community for psychiatric patients with severe mental disorders in the Marche Region, a research study was conducted (Sagripanti 2021) in which six patients were enrolled and given a narrative protocol for the duration of 16 weeks in parallel with a control group of the same number of subjects who continued their usual rehabilitation process. The narrative protocol provided that each person recounted his or her own experience about a specific topic previously chosen together with the whole group; during the story the other members could listen and ask questions to the narrator without, however, presenting their own content. Each topic therefore involved six storytellers for six meetings that made up each session. The meetings were facilitated by a professional educator. At the beginning, during and at the end of the study, the two groups were given Rating Scales relating to clinical progress (BPRS); to the evaluation of the effectiveness of the intervention (CGI); to global functioning (GAF); to the quality of life (EuroQl) that allowed a quantitative evaluation of the evolution of all participants, while the group of narrators was also proposed a narrative questionnaire not yet validated but capable of collecting qualitative data; finally, a free text was requested on the lived experience.
I report the one of one of the narrators: male, 50 years old with a diagnosis of Paranoid Schizophrenia with continuous course (DSM V criterion F20.9); history of illness lasting about 30 years: “We were strange guys, each one immersed in his own problems, it was not easy to understand what made us suffer but we all wanted a happy future or friendship or couple but always with the wind in our sails. Unwittingly, after going around different departments, we all found ourselves in a community where each of us had to try to renew ourselves”.
On a qualitative level, through the tools of Narrative Medicine, we can see a narrative centered on the experience of illness, to the “illness” understood by Kleinmann as “the meanings attributed by the person to his health condition/experiences and experiences related to his health condition” (Covelli V. 2017), which at the same time, is placed in Frank’s quest narratives such as: “(…) People who narrate in this way have control of their lives even if their health condition will not improve (…) and wish to share their story with other people in order to help others who are experiencing the same condition” (Covelli V. 2017) . On a quantitative level, the rating scales showed an improvement in BPRS scores predominantly regarding affective flattening. The CGI showed an increase in the efficacy index; the GAF an improvement in global functioning and the EuroQoL an improvement in perceived quality of life. The qualitative and quantitative results are integrated in a coherent way, indicating a clinical improvement parallel to the increase of a narrative capacity capable of expressing unsuspected resources of great potential in terms of personal evolution.
This is suggestive of a specific property of narrative as a rehabilitative tool capable of reactivating the affective resources that the serious pathology had compromised but not extinguished. Consistently Ciompi sustains the presence of “[…] an affective-cognitive binary, which in childhood and youth was clearly nourished by a great affective interest, but then was apparently emptied in the general flattening of feelings of chronic psychosis. The fact that one can manage to reactivate such a hidden binary of feeling, thinking, and behavior after a latency of many years also reveals that the considerable reserves of affectivity or, rather, energy, even in such sufferers can remain hidden under a thick shell of indifference” (Ciompi, 2001). The telling of the story reactivates the hidden binary through that particular mental state described by Morin as “a mimetic capacity of psychism that supposes a second state that I call semi-trance, in which the unconscious and consciousness cooperate. (…) The author is not necessarily aware of what his work contains because this work comes from a second state in which creativity has overtaken his consciousness” (Morin, 2019). This happens not only to the novelist but also to anyone who writes and notices it when they happen to reread their own writing after years. The text and the results of this work depose the effectiveness of the narrative approach in patients with severe mental disorders and the validity of integrating the quantitative tools of EBM with the qualitative ones of MN in order to be able to access with greater appropriateness the natural complexity and the evolutionary dynamics of the sick man. During the lockdown period in which the study was conducted, no flare-ups occurred, no changes in drug therapies were required, and all subjects involved presented documented clinical improvement rather than the expected worsening due to pandemic stress (Kozloff, 2020; Sánchez-Guarnido, 2021).
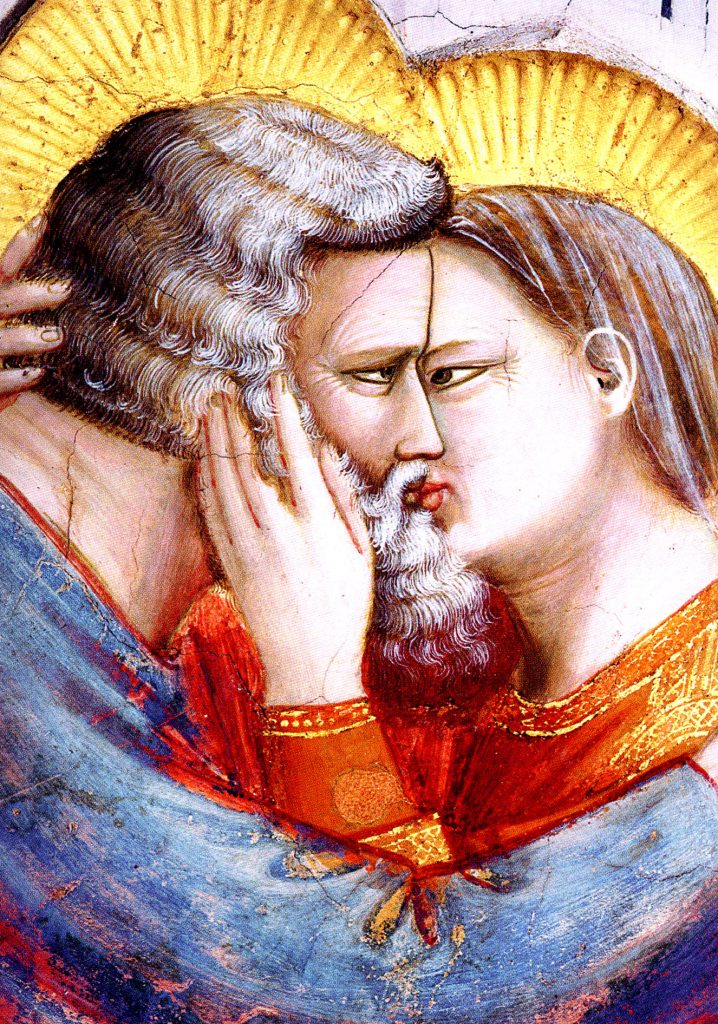
This modest contribution is intended only as a hypothesis of research in psychiatry, or at least, of doubt about knowledge: “or I do not know who put me in the world, nor what the world is, nor what I myself am; I find myself in terrible ignorance about all things; I do not know what my body is, what my senses are, what my soul is, and this very part of me that thinks what I am saying, that reflects on everything and on itself, and does not know itself just as it does not know other things” (Pascal 1670). Atoms split and merge releasing enormous energies, Particles dance; men are composed by them, but the story of every mind starts almost always from a Kiss.
Article by Dr. Ubaldo Sagripanti, Psychiatrist
- 1) American Psychiatric Association (2013). DSM-V – Manuale Diagnostico e Statistico dei Disturbi Mentali, Raffaello Cortina Editore, Milano 2014.
- 2) Cambridge Dictionary https://dictionary.cambridge.org/dictionary/english/mind
- 3) Ciompi L. (2001). I fondamenti emozionali del pensiero. CIC Edizioni Internazionali.
- 4) Covelli V. (2017). Approcci, metodi, disegni, strumenti: il punto di partenza per una riflessione metodologica. In Covelli V. (ed) Medicina Narrativa e Ricerca. Libellula Edizioni
- 5) Hustvedt S. (2016). Le illusioni della certezza. Einaudi 2018
- 6) Kozloff, N., Mulsant, B., H., Stergiopoulos, V., Aristotle, N., Voineskos, A., N. (2020). The COVID-19 GlobalPandemic: Implications for People with Schizophrenia and Related Disorders. Schizophr Bull, 8;46(4):752–757.
- 7) Morin E. (2019) sull’Estetica. Raffaello Cortina Editore
- 8) Pascal B. (1670). Pensieri. Bompiani 2000
- 9) Sagripanti U., Pietracci S., Paolucci C., Scipioni B., Divisi R., Monterubbiano M. (2021) Effectiveness dell’intervento narrativo sulle dimensioni psicopatologiche e sull’evoluzione clinica di pazienti psichiatrici residenziali durante la pandemia da COVID-19. Psichiatria e Psicoterapia (2021) 40, 4, 176-198
- 10) Sánchez-Guarnido, A., Hidalgo, N., Arenas de la Cruz, J., Esteban, I., Mondón, S., Herruzo, C. (2021). Analysis of the Consequences of the COVID-19 Pandemic on People with Severe Mental Disorders. Int J Environ Res Public Health, 13;18(16):8549.
- 11) Treccani Enciclopedia. https://www.treccani.it/enciclopedia/psichiatria/
