THE FOREWORD
The life of health organisations
Saving the common good
In the media, after the long post-Covid silence, we are back to talking about healthcare. The news that reaches us is that of differing visions between health workers and the government on early retirement, of one doctor out of two in burn out (52%), a percentage that drops only slightly for nurses (45%, data from Sole 24ore Sanità, 2023).
From heroes applauded on balconies to today’s ‘scarce’, ‘precious’ and ‘senior’ resources: the closed number of the last twenty years and the short contracts, the COVID -19, the increase in the age of the population, the increase in mental illness post COVID and from war conflicts in Europe have meant that ‘the medical and nursing class’ has to review and rethink the rules of its professional life inside and outside the organisation to which it belongs.
In an attempt to shed light on life inside healthcare organisations, ISTUD Sanità e Salute designed and carried out between December 2023 and January 2024 the quantitative and narrative research “Life in Healthcare Organisations.” For the numerical part, we drew on Cristina Maslach’s questionnaire to assess the risk of burn out in the three dimensions of Depersonalisation, Emotional Exhaustion, and Realisation, prepared back in 1981
(the Maslach Burnout Inventory). For the qualitative part, very simple stimuli were used that invited narrative such as “I feel…”, “I think…” and “I want…” “The others who work with me…” The people I care for…”.
Through this research, the motivations, energies, needs and quality of care in the perceptions of professionals were investigated.
THE SOCIO-DEMOGRAPHIC RESULTS
176 people took part in the research, with an average age of 52 years: this figure is consistent with the ISTAT figure for collaborators in the public administration, 51.8 years (this means that the research reached the desired target), with a range of ages from 25 years of newly graduated doctors now in specialisation to 77 years of those who still collaborate within the health service.
With the same stratification of contacts sent in the different regions, and asking for the research to be sent also to colleagues who had never undergone training on “soft skills – communication, narration”, the North responded with 65.9%, perhaps demonstrating that participatory activism that wishes to shed light on the situation in order to speak out, the Centre at 19.1% and the South at 15.8%. It should be noted, however, that the first region in terms of responses was Lombardy, second was Piedmont, third Sicily, and fourth Lazio, with Tuscany and Veneto. 73.9 % of the narrative and quantitative answers came from women, 25.5 % from men, and 0.6 % wrote other.
The data from the WHO 2019, indicate that in Italy 70 % of the care professions are performed by women, and in this sense, albeit with a slightly higher percentage, the research is in line with this figure. For the health professions, 44.4 % are medic*, 43.3 % are nurses*, while the remaining 12.3 % are psychologists*, physiotherapsists*, speech therapists*, and other figures working in healthcare.
THE RESULTS OF THE MASLACH TEST ON BURN OUT
THE RESULTS OF THE MASLACH TEST
We investigated whether the Burn Out test, which is based on three main domains such as Depersonalisation (D, i.e. detachment from the patient in care, coldness, alienation, lack of empathy), Emotional Exhaustion (being exhausted by both emotional load and workload), and Personal Achievement (R, gratification, recognition, being able to make decisions independently) is so detective of the state in which professionals in the National Health Service find themselves. Here is a very summarising and highly polarised table of the Maslach test: the questions with the always and never answers, the range and the burn out risk index: remember the three spheres of the test (Depersonalisation, Emotional Exhaustion, and Realisation)
| field | question | always | never | risk index |
| depersonalisation (resonates with EE) | I feel emotionally envolved with patients | 40% | 2.6% | very low |
| realisation | In the evening I feel like an object | 11% | 11% | high |
| emotional exhaustion | i feel tired in the morning | 13% | 19.7% | medium |
| depersonalisation | I empathise with patients | 21% | 2.4% | low |
| depersonalisation | Patients as objects | 2.6% | 52.3% | very low |
| emotional exhaustion | stress with people | 3.5% | 21.1% | very low |
| realisation (resonates with D) | Coping well with patients | 21% | 2.6% | low |
| emotional exhaustion | I feel consumed by work | 15% | 15% | high |
| realisation | I feel positively influenced by the experience of others | 12% | 8.6% | medium |
| depersonalisation | greater insensitivity | 4,7% | 42,8% | very low |
| depersonalisation | I am hardening | 4.6% | 23,7% | low |
| emotional exhaustion | I feel full of energy | 8,6% | 9,9% | very high |
| realisation | I feel frustrated | 10.2%, follows 13.2% | 23% | high |
| depersonalisation | I do not care about the fate of my patients | 0.5% | 71,1% | very low |
| emotional exhaustion | I feel like I work too much | 18%, follows 21,9% | 8,6% | high |
| emotional exhaustion | Working with people is stressful | 11.2% | 8.6%, segue 17,8 | high |
| depersonalisation | I create a relaxed atmosphere with the patient | 23%, follows 33% | 2% | very low |
| emotional exhaustion | Exhausted after day with patients | 13.2% | 11.2% | medium |
| realisation | Gratifications from work | 23% | 6.6% | low |
| emotional exhaustion | I am on the edge of an abyss | 3.5% | 46.7% | very low |
| emotional exhaustion | I solve emotional problems calmly | 19% follows 27% | 2.6% | very low |
| depersonalisation (resonates with EE) | Patients vent to me | 21% | 5.3% | very low |
These are the summary results of the polarisation of responses. The indications are many, and certainly to be intersected with the narrative fragments. But even in stand-alone mode they give us a compass of the possible burn-out of healthcare in Italy.
Depersonalisation, i.e. treating the patient as an object, cynicism, slow violence towards patients, the absence of empathy, the brutality of these responses is just a very remote hypothesis: on the contrary, the mission of care is ‘sacred, untouched’, patients are listened to, they can vent, they are welcomed with their emotions, logical plans for their care are thought of. And perhaps it is from talking to patients that the fundamental energy is created to move forward in the health care system by creating a Common Wellbeing between patients and health professionals. On this front the risk of burn out is not really infinitesimal. Even in the narratives of “I want to…” Patients are at the centre:
- Continue to do the best I can do
- continue the collaboration as long as it is possible for the organisation and can be reconciled with my other commitments.
- I want to treat
- possibly be helpful
- continue to love this job
- Leave my know-how to the younger generation and my passion for my profession, which cannot be separated from the knowledge that a helping profession is CHOSEN and that it is at the service of people
- Doing my best
- I would like to create a welcoming, creative, professionally stimulating atmosphere. I would like skills to be evaluated for results, also listening to patients’ opinions, I would like less bureaucracy. I just want to work doing what I studied for with passion
- I want to be there. And find the best way. It is not others who give us satisfaction. I find it in looks and gestures. And in the relationship which is not always positive but I look for it to be so. I would like it to be so
- To continue this work, implementing the aspects of information and support for families and training for health workers
- To continue to always do my best towards patients
Emotional Exhaustion almost never results from the related questions with the patients, whose risk is low, but from the system, with the fatigue, the fatigue, the energy required, which is no longer a human load, but becomes inhuman. So even the concept of Compassion Fatigue , fatigue from too much compassion with patients is put into crisis, compassion paradoxically is energy, it motivates, it makes one give one’s best, it does not exhaust. Energy is undermined by routine, that “I feel tired in the morning”, which should instead be the moment when we ask ourselves “how can we contribute with our work today?” Stress responses with colleagues (people) do not seem so polarised. On this front, the risk of burnout was identified in workloads (I feel consumed by work) and this is where remedies need to be put in place immediately that go far beyond the satisfaction of daily budgets.
With respect to the narrative invitation “I feel…” here are some verbatim underlining fatigue:
- overwhelmed, exhausted, lifeless. Everything that used to give me pleasure in my work now weighs a ton. Whereas before I would stay extra hours if I needed to, now I can’t wait to escape
- …struggling from an ethical point of view, aware of being limited in the possibilities of care by bureaucratic practices and by medicine administered and not practised according to true needs
- Constantly suffering from increasingly demanding workloads with a high level of responsibility, perpetrated demotion due to the chronic shortage of professionals
- Incomplete, with the many staff and material shortages. Overworked, given the profuse incompetence and/or unavailability of colleagues/staff
Realisation is apparently ambivalent in that it is composed of self-realisation through the maturation of one’s own competences, and the absence of recognition by others: many feel frustrated, not understood, but are the same as those who feel good, self-esteem, are full of gratification given by patients, and their own increased knowledge. The risk of burn out, although no one is on the brink, lies in the theme of frustration due to lack of gratitude from management (and not from patients and colleagues). Here are some written testimonies that reveal this sense of Malaise – the narrative invitation was “I feel…” and Well-being.
- Undervalued for acquired skills, personal qualities and resources, not involved in projects despite availability and titles
- Tired as if I were fighting windmills, undervalued most of the time especially when something needs to be changed, public health no longer puts the health of the citizen at the centre so frustrated
- Underpaid for my professional skills. Underpaid for the responsibilities I take on. Little or no protection from a medico-legal point of view. Frustrated for not seeing clear career possibilities.
- Often stifled by demands and things to do. I also feel useful when I can help people or colleagues in need. Lately, I experience a sense of helplessness because of the difficulties of health professionals and the discomfort of patients in front of waiting lists.
- Fatigued, not valued, not adequately remunerated
- Mobbed and put under pressure Coordinated by people who do not understand (through ignorance and haughtiness) my role and my work
- Very well received, there is a familiar and smiling environment, a lot of personal autonomy and great appreciation for what everyone does and manages, without rivalry as was the case in the previous workplace I came from (university hospital)
- Constantly insecure about my future and the possibility of professional growth. Unable to plan holidays or well-earned time off. Tired and exhausted. Happy with results and patients’ appreciation. Useful to patients. Esteemed by colleagues and patients
- I have an experience of ambiguity, on the one hand I am happy because I do the work I like. On the other I feel misaligned with what the NHS is proposing today, the person is no longer at the centre, there are economic and market interests. This is not the public health care that I helped to create
- Very good but very fatigued by the responsibilities and pressure from regional institutions that demand data without assessing the quality of care provided because they rely solely on checklists
The results of Maslach’s test on burn out, designed back in 1981, show how far health professionals have come in embracing the need to be empathetic, compassionate without effort, learning to embrace patients’ emotions and making it their strength, no longer their weakness: and this result at a time when the Italian projects we are aware of are called ‘Save the National Health Service’.
The attitude of our participants makes us realise how much, once the willingness to profess care is embraced, it becomes part of the person’s identity, epi-genetically transforming his or her DNA. The themes of caring, patient-centredness, compassion, inclusion are here on the table, and in great development in 2024.
The danger lies in the abuse of this profession of caring by management systems, (not leadership), precisely because they are often ‘Good’ people, even too ‘Good’. People who do not know how to set limits and hurt themselves, not because of the pains and illnesses they cure, but because of the too many yeses out of submission they say to higher hierarchical positions (some with little reflection, and little natural intelligence). Submission comes at the expense of motivation, and this is an issue that needs to be addressed for leadership to become wiser and more mature. And leadership that is absent-minded and short-sighted and not of service jeopardises the production of the Common Good.
NARRATIVE RESULTS
NARRATIVE STIMULUS I FEEL…
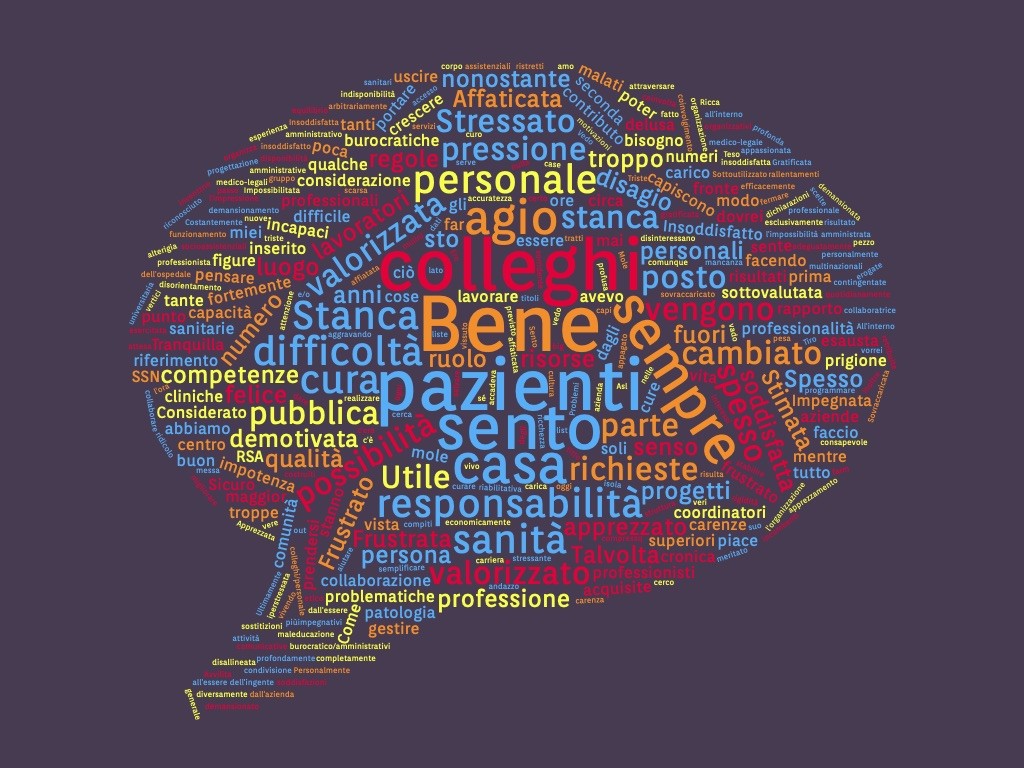
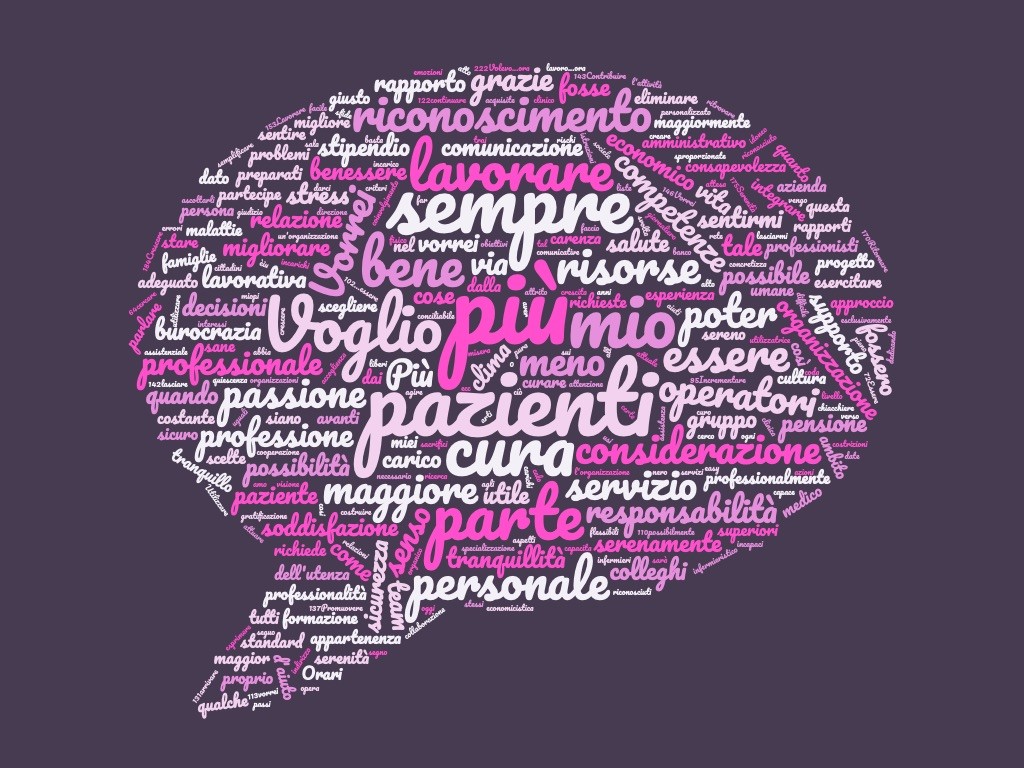
Figure 1 Word Cloud of “I feel…”
In this section of our anonymous and voluntary narrative survey, we asked doctors, nurses and healthcare professionals how they feel about working in their organisation. What you find listed below are some narrative fragments we selected from all those sent to us.
In the word cloud “I feel” is clearly central, but not only: “colleagues”, “staff”, “responsibility”, “home” “tired”, “difficulties”, “pressure “are also particularly recurrent.
I FEEL.
NARRATIVE FRAGMENTS OF SATISFIED EASE (34/153, 22.2%)
Here are some examples:
- At ease
- Good. It is pretty much like any administrative office outside the hospital
- …being able to contribute to the system, improving procedures and quality of patient care
- …myself. I can freely express my ideas, and they are considered and scrutinised.
- …to be part of a community. We are a small group of professionals who deeply love this work and thanks to deep sharing and planning that takes into account personal aptitudes, we have the opportunity to grow and provide caring relationships that are effective, personal and that help the person find motivation and tools to get through what they are experiencing.
- Good. Because it has always been my life and I have always sought the place where I felt best. The place that belonged to me
NARRATIVE FRAGMENTS OF PARTIAL EASE (13/153, 8.5%)
Here are some examples:
- Peaceful. The work is certainly very stressful in itself, but one does not feel lonely
- Very well received, there is a familiar and smiling environment, a lot of personal autonomy and great appreciation for what everyone does and manages, without rivalry as was the case in the previous workplace I came from (university hospital company)
- I changed jobs and location two years ago. I was in burnout. Now for 2 years I am fine
- A reference, a support for people with pathologies, a collaborator for other colleagues, an asset for the company. I feel busy more than I would like, but I try to manage work time and personal time with balance. Even if I sometimes feel I am taking time away from my personal life.
- Satisfied, motivated to make my contribution to improve the care processes of the people who come to DSM-D. Sometimes, in the face of limited resources that force me to make choices that are not always optimal, my enthusiasm ‘cools down’ but only time to study new strategies to bring home the result. I strongly feel the need to break out of habitual patterns because I am convinced that only in this way can we save our NHS
AMBIVALENT NARRATIVE FRAGMENTS (27/153, 17.7%)
Here are some examples:
- Tired but satisfied
- Rich in experience but uncomfortable with ever-increasing administrative and bureaucratic demands
- Sometimes I feel like I am in a second home, and inside all homes one feels differently depending on the day and time
- Within a fairly close-knit team but embedded in a context in which it is increasingly difficult to move around effectively
- Like at home. Problems and satisfactions, limited resources, inventiveness, competence, connections. Like at home
- Sometimes at home. Sometimes in prison.
- Constantly insecure about my future and the possibility of professional growth. Unable to plan holidays or well-earned time off. Tired and exhausted. Happy with results and patients’ appreciation. Useful to patients. Esteemed by colleagues and patients
- I have an experience of ambiguity, on the one hand I am happy because I do the work I like. On the other I feel misaligned with what the NHS is proposing today, the person is no longer at the centre, there are economic and market interests. This is not the public health care that I helped to create
- Very good but very fatigued by the responsibilities and pressure from regional institutions that demand data without assessing the quality of care provided because they rely solely on checklists
- …at ease with the skills I have acquired over time and the interest I still have in the profession; often exploited on shift work and requests for substitutions that I feel I should no longer have to bear; imprisoned by the impossibility of getting out of the condition of shift worker
- Often overwhelmed by demands and things to do. I also feel useful when I can help people or colleagues in need. Lately, I experience a sense of helplessness because of the difficulties of health professionals and the discomfort of patients in front of waiting lists.
NARRATIVE FRAGMENTS OF PARTIAL DISCOMFORT (13/153, 8.5%)
Here are some examples:
- I went from being enthusiastic to being exhausted
- Sometimes in a blender, too full and too fast
- A fighter, often struggling to spread the rehabilitation culture
- Since retirement I have been working in private health care and in an elderly residence RSA. I see growing disorientation over the delayed responses of public healthcare. Those who have no money give up on care. The RSAs are taking over from the long-term care facilities. I feel like the end of an era
- …ethically distressed, aware of being limited in the possibilities of care by bureaucratic practices and by medicine administered and not practised according to real needs
NARRATIVE FRAGMENTS OF TOTAL DISTRESS (66/153, 43.1%)
Here are some examples:
- Endangered
- Without prospects
- A piece of a gear whose operation is intended to produce wealth for the organization rather than to take care of users
- Since after covid, everything has changed. We’ve become numbers, which directions use for “projects.” Every day there is some more bureaucratic menace that takes away time of care. Personally, I am disappointed with this new gait. Leaders and heads have been created who invent rules and do not care about the well – being of staff and patients. I’m shooting, which I’ve never done before, doing my job and not wasting energy that’s so untested. I feel like I’m working like a worker and not like a professional
- Abandoned by the company, alone.
- Unprotected
- Not valued. I feel like a pawn to fill the shift box. Professionalism and training are not valued in any way
- …betrayed and I often feel a sense of strangeness
- My profession is always undervalued even within the hospital health sector. We are the professionals who most of all welcome and listen to the sick because we are the ones who have access to their spirit as well as to their body, the patients, with us confide and always expect us with many requests. On the other hand, health companies are incapable of taking care of people, aggravating the feeling of helplessness of those who try to do their best. Here in Veneto, despite the many declarations of intent, the services are being depleted more and more. Moreover, those at the top of the command pyramid (but also the department coordinators themselves) are incapable of making the workers of the real teams. It seems that patients and workers are just numbers that health companies are not interested in …
- …saucepan sauce
- …overwhelmed, exhausted, unconscious. Everything that pleased me in my work now weighs a quintal. While I used to stop for extra hours if it was needed, now I can’t wait to escape
- Poorly valued for acquired skills, qualities and personal resources, not involved in projects despite availability and titles
- In constant suffering for increasingly demanding workloads with high responsibility, remanding perpetrated for the chronic shortage of professional figures.
- Incomplete, with the many shortages of personnel and material. Overworked, due to profound incompetence and/or unavailability of colleagues/staff
- Mobbized and pressurized. Coordinated by people who do not understand (by ignorance and haughtiness) my role and my work
- Tired as if struggling with windmills, undervalued for most of the time especially when something needs to be changed, public health no longer puts the citizen’s health at the center of frustration
- Underutilized for my professional skills. Underpaid for my responsibilities. Little or no medical protection. Frustrated not to see clear career prospects
- Fatigued, undervalued, underpaid
Below is a graph of the total of 174 participants in the survey 153 who have left their testimony in this specific section, “I feel…” (about 88% of the total).
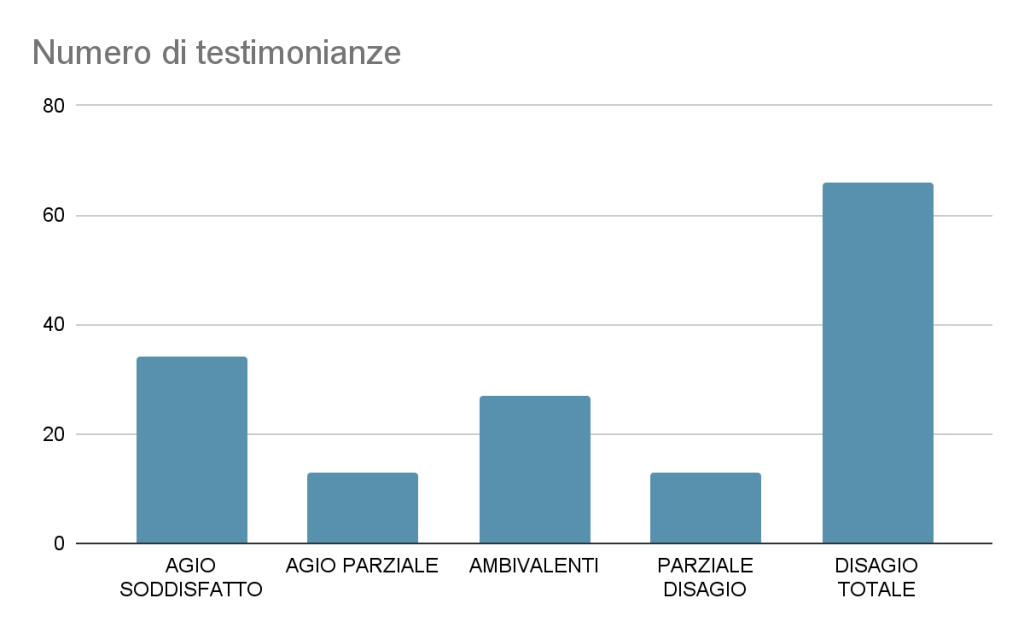
Figure 1: types of responses to the narrative stimulus “I feel…” and numerical frequency (n=153)
From the testimonies collected, a complex and nuanced picture emerges, in which there is a progressive increase of dissatisfaction with the current state of affairs. However, in parallel to this finding, there is a significant and palpable determination to improve the current status quo. Several facets of job satisfaction clearly emerge among the participants: from those who declare themselves fully satisfied in their role, to those who complain of underestimation of their skills and to those who live a sense of ingratitude towards their commitment. The emotional complexity of this situation is reflected in ambiguous and ambivalent feelings involving many people involved.
It is interesting to note that the participants, far from merely describing their emotions, chose to narrate their working condition with scrupulous precision and forthrightness. This open and sincere approach enriches the picture, providing a detailed and authentic view of the different realities experienced.
It is clear that, apart from a few isolated cases, love for one’s profession is a stable and constant factor, regardless of whether one’s employment situation has been assessed positively or negatively. This phenomenon underlines that, beyond the challenges and difficulties, the prevailing sentiment among Italian health workers is characterized by a deep and deep-rooted determination to pursue their role with commitment and dedication.
NARRATIVE STIMULUS I THINK…
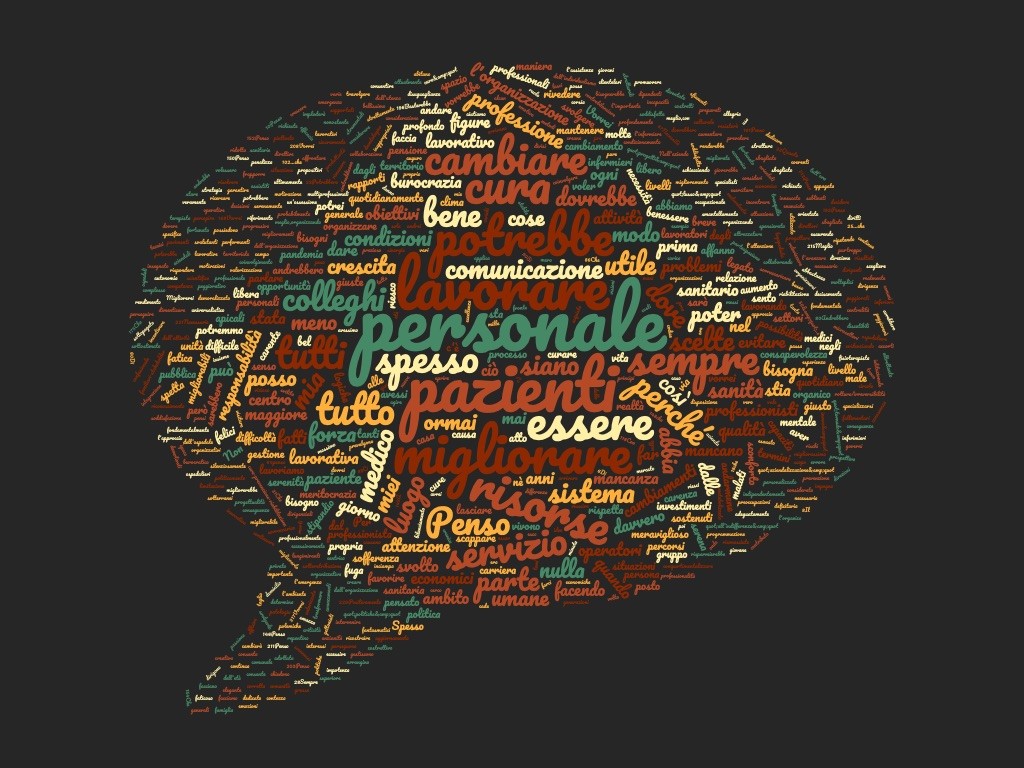
Figure 2 Word Cloud answers to the narrative stimulus “I think…”
In this section of our anonymous and voluntary narrative survey we’ve asked doctors, nurses and health care professionals what they think about the work they do in their organization. What you find listed below are some narrative fragments that we have selected for you from all that have been sent to us.
The word cloud focuses on the theme of “staff”, along with “resources”, “change”, “improve”, “could”, “work” “useful and good” (these are areas of rethinking possibilities).
I THINK…NARRATIVE FRAGMENTS OF SATISFIED EASE (21/150, 14%)
Here are some examples:
- How useful and wonderful the work of the rehabilitation staff: physical therapist, speech therapist, occupational therapist
- That it was lucky to meet people and themes that give me a lot
- To my work, how to improve myself and the working environment to ensure a superior service
- To go on doing the best according to method, knowledge and listening and continuous opportunities for growth
- That I have found a place where I can plan for the long term and bring in people I trust and have worked with in the past profitably and that I currently know I am not happy or satisfied in my own work system because of technical problems or failed management choices
- May there be space to work with humanity, making the relationship a precious time of care
- That makes me happy
- That I’m lucky to work with a good group
NARRATIVE FRAGMENTS OF PARTIAL EASE (9/150, 6%)
Here are some examples:
- I’m retired. I work in private and I don’t feel bad. Here too, it is important to create a communication network for multiprofessional synergies. But if you’re wise, you can do it, and it’s even better than institutional research.
- that health care is often of the highest standard, when it expires it is linked to resource constraints, inability to engage and motivate, lack of updating and communication
- I think it would take serenity and joy because we are often overwhelmed by the suffering that takes us deeply but we cannot get overwhelmed. If we help, it’s better.
AMBIVALENT NARRATIVE FRAGMENTS (26/150, 17.3%)
Here are some examples:
- I think seeing so many sick people and so much suffering sometimes burdens you with emotions that you struggle to dispose of. But in the end you think tomorrow is another day
- That we could work better if everyone really wanted to work together, collaborating between the different professional figures. That we’re a nice working group, young, respecting each other, but lately paying for management’s choices
- i will never regret having chosen this beautiful job but unfortunately it is increasingly difficult to carry it out well; there is a lack of human resources and often also of instrumental resources; there is a lack of the right skills in the key areas where decisions are taken and vision for the future is missing
- I think my job as a hospital doctor is wonderful but definitely underpaid now and probably even once I retire. I think that the flight from hospitals is increasing and will get worse over the years because it is not enough passion to balance under-pay, workloads, burden of responsibility and legal medical risks. I think that the public health system is in difficulty because of governments’ unfocused and farsighted choices, and this penalizes doctors, nurses and patients
- That it has been and still is a place of excellence, many great doctors have left, I feel very discontent in all sectors.I think I’ll be short-lived. I’m planning to change jobs.
NARRATIVE FRAGMENTS OF PARTIAL DISCOMFORT (56/150, 37.3%)
Here are some examples:
- That it will be difficult for the new generations to maintain a good working climate with the changes taking place
- My service should be more integrated with other specialists so that we can really talk about care
- That there needs to be an innovative push that puts people at the center of everything, both professionals and users
- That we could organize time and resources better, that often of all the effort and effort that we put into action only a small fraction emerges
- That people make a difference, that they can put a brake, a limit on excessive or completely inconsistent demands
- That there are the capacities and possibilities to do well, but we are not in a position to carry out our work in a correct, serene way.. all this is the fault of the wrong management and the policy put in place by the city councilI wish I could help to improve it, I hope I have the strength to be able to continue to fight, a strength that is being exhausted to give way to despair and a confused state of mind
- Patients’ rights are sometimes overshadowed by company policies that have few staff and overburden individuals with multiple activities to make up for a shortage of other staff. The consequences over the years on the physical and the psyche create new sufferers. The work has become so worrying that I can no longer perceive the noble end.
- I think that communication with patients is very poor on the part of many professionals who also have excellent technical skills. I think that the multiunit mobility strategy adopted for nurses to tackle chronic staff shortages does not relate anything to the quality of care because it does not allow professionals to specialize in a specific area.
- That where I work now is a “luxury” that not everyone lives in their working career. The reality is that we are being asked to spend less and less time on what we do. In all this, the responsibilities are high, as is the risk of error. What is frightening is the awareness of all this and that the more time passes and the less improvements are seen, increasingly enveloped by a “tornado” of bureaucracy
NARRATIVE FRAGMENTS OF TOTAL DISCOMFORT (38/150, 25.3%)
Here are some examples:
- To leave
- Wanting to go away
- That will implode shortly
- I’m only here because I have to work. I’d like to run away
- That I’d like to change jobs
- i often think i’m quitting my job as a doctor for a job that allows me to be more carefree, especially when i leave work, a job that doesn’t leave me worry when i’m at home
- There is no hope
- I think if I had to choose to change my life to be well right now I would go to another profession
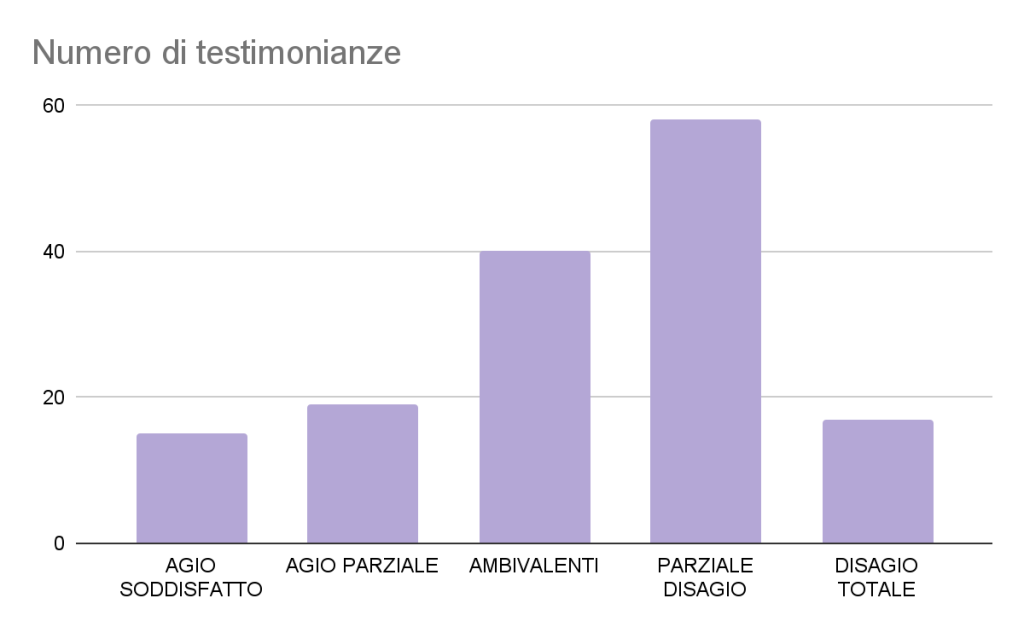
Below is a graph of the total of 174 participants in the survey 150 left their testimony in this specific section (about 86% of the total).
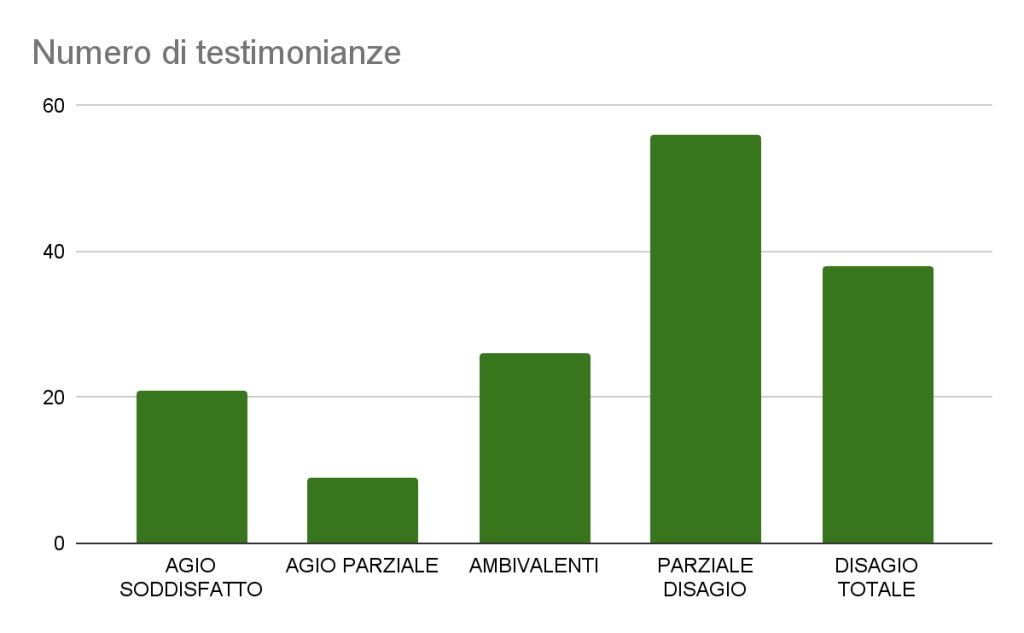
Figure 2: Types of responses to the narrative stimulus “I think…” and numerical frequency (N=150)
The difference with the previous section “I feel…” in which we asked our volunteer participants to leave a testimony of their emotions and feelings is evident. While in that section of our survey there was for the most part a feeling of great despair (witnessed by the high percentage of responses that can be included in the category NARRATIVE FRAGMENTS OF TOTAL DISCOMFORT), now the picture is different. The predominant category this time is that of NARRATIVE FRAGMENTS OF PARTIAL DISCOMFORT. That is, when our participants were asked to switch from the emotional and sensory (I feel…) to the rational (I think…) plan, a change of perspective occurred. Criticism of the system has remained, but in most cases has gone from being destructive to being constructive.
The reflection on this situation clearly indicates that, despite the pervasive nature of the discomfort, there are signs of a possible positive transformation. Individuals involve their critical and generative thinking more in the process, which could open the way to constructive solutions.
However, the prevalence of those who express the desire to completely change profession raises a red flag. This information underlines the depth of the discomfort and the need to address the challenges more comprehensively and effectively. It is essential to explore options and resources that can support these individuals in pursuing positive and lasting change in their professional lives.
NARRATIVE STIMULUS I WANT…
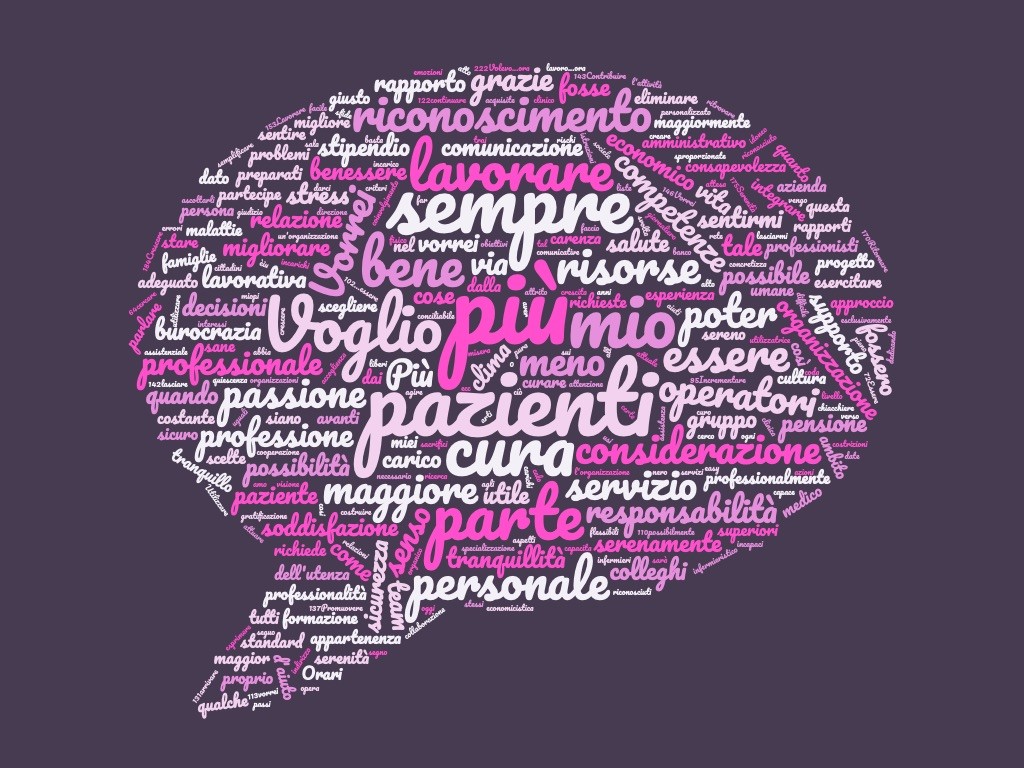
Figure 3 Word Cloud of the answers to the narrative stimulus “I want…”
In this section of our anonymous and voluntary narrative survey we asked doctors, nurses and health care professionals what they would like to change in relation to the work they do in their organization. What you find listed below are some narrative fragments that we have selected for you from all that have been sent to us.
In this cloud of words, the important role that the word “more” assumes is interesting (which may indicate not wanting to work anymore or even the opposite wanting to do more). Interesting also the role that words like mine, patients, passion, resources and recognition assume (you would like more recognition…). But also less bureaucracy. As always, the word cure is central to the vocabulary of our professionals.
I WANT TO…NARRATIVE FRAGMENTS OF SATISFIED EASE (15/149, 10%)
Here are some examples:
- Keep doing the best I can
- continue the collaboration until it is possible for the organization and reconcilable with my other commitments.
- Nothing more
- I want to cure
- possibly help
- keep loving this job
- Leaving my knowhow to the younger generation and passion for my profession which cannot ignore the awareness that a helping profession is CHOSEN and that it is at the service of the people
- Do my best
NARRATIVE FRAGMENTS OF PARTIAL EASE (19/149, 12.7%)
Here are some examples:
- I would like to create a climate of welcome, creativity, professionally stimulating. I would like skills to be assessed for the results achieved, and I would also like to hear the opinion of patients, and I would like less bureaucracy. I just want to work doing what I’ve studied passionately for
- I want to stay there. And find the best way. It is not the others who give us satisfaction. I find it in looks and gestures. And in the report I do not always look for good, but I look for it. I wish it were
- Continue this work, implementing information and family support aspects and training for healthcare professionalsAlways keep doing my best to patients
AMBIVALENT NARRATIVE FRAGMENTS (40/149, 26.8%)
Here are some examples:
- I’d like to work in peace. I do a job that I love and that I continue to do thanks to the gratifications given by the patients that I treat, certainly not for the meager pay or no recognition given me company and superiors (primary)
- I want to be able to work calmly, without bureaucratic constraints and harassment dictated by an exclusively economical view of health; I want to make time for training, new stimuli to integrate the scientific aspect of medicine with the human one; I want to improve my communication and empathic skills more and more
- Have a work organization that is attentive to the wellbeing of its employees. I would like to remove from the bureaucrats who govern us the most incapable and shortsighted people who, unfortunately, hold positions of leadership with salaries that are completely disproportionate in excess of their actual performance.
- A serene and proactive climate, collaborative. I wish that people who only think about their personal interests, polluting and devastating a public service, were turned away. An apple rotts among the healthy apples, makes the others rotten
- …remain committed to patients but also no longer be harassed by constant blunt decisions by incompetent
- I prefer, “I’d like.” Perhaps a more relaxed environment and a more courteous and moderate attitude on the part of users. Even more reasonable and informed.
NARRATIVE FRAGMENTS OF PARTIAL DISCOMFORT (58/149, 38.9%)
Here are some examples:
- hope that something will change, because it is no longer sustainable
- I would like to see greater involvement of operators and citizens, greater awareness of the risks we are all taking. If the Public Service collapses, diseases and discomfort will increase, because of a decline in prevention and treatment and for the lack of protection of one of the primary resources to be in the world and to realize one’s life project: health, which I understand as such even when there are disabilities, chronic diseases etc. Health is feeling that you can face the challenges of life with personal resources and family and social network. Health is perceived to be well-being, not a standard given from the outside
- Have more time to think about how to help people heal, instead of treating their symptoms and so on
- To have a healthy approach rather than a pathogenic one, to be able to promote the possibility of intercepting health not only at the physical level. Use different languages and care tools to help reduce stress and process emotions. I want to support the report as a time of care, not just with the users. I want reflection, clinical reasoning, to be considered by every colleague as essential to action, which is not so obvious.
- More consideration for those who work well, more independence from doctors, greater professional recognition and a salary equivalent to European nursing standards
- More consideration from the Management, which seems to be ignorant of the constant shortage of staff and requires us more and more efforts, also from the users, who rightly require a suitable service and is increasingly angry about the very long waiting lists, not understanding that most of the services go ahead for our good will and dedication to our work.
NARRATIVE FRAGMENTS OF TOTAL DISCOMFORT (17/149, 11.4%)
Here are some examples:
- Do I want? I want to hold out until I retire.
- I want to go away
- quit work
- Changing the workplace
- Go awayI just… I’m just doing mine
Below is a graph of the total of 174 participants in the survey 149 left their testimony in this specific section (about 85.6% of the total).
Graph 3: Types of responses to the narrative stimulus “I want…” and frequency numerics (N=149)
In this specific section of the analysis, there is a noticeable increase in the number of responses, which are attributable to the category of ambivalence and partial discomfort. This significant increase in participation by our interviewees provides an indication of their readiness to examine clearly and carefully the various opportunities for implementing improvements. This emerging willingness becomes apparent when participants are encouraged to openly share their testimonies about what they would like to see implemented in terms of changes in the organizational structures of the health sector in which they actively pursue their profession. More importantly, the evidence obtained is that health professionals are clear in identifying not only possible problems, but also in putting forward thoughtful and concrete solutions.
Complaints of absolute discomfort have greatly diminished and total discomfort has become partial or ambivalent. Asking our participants what they want triggered a stimulus to design that contained destructive critical content and sense of frustration.
THE NARRATIVE STIMULUS TO OTHERS WORKING WITH ME…

Figure 4 Word Cloud of the replies to the narrative stimulus “Others working with me…”
In this section of our anonymous, voluntary narrative survey, we’ve asked doctors, nurses and health care professionals what the relationship is with their colleagues. What you find listed below are some narrative fragments that we have selected for you from all that have been sent to us.
In the cloud of words, the words “tired” and “all” are certainly struck, together with “fatigue” in such a prominent position; however, the analysis carried out in the other sections also shows that this fatigue does not result from burnout but from structural problems in the organization in which they work. The role of demotivated (and demotivated) and stressed words is also important.
THE OTHERS WHO WORK WITH ME…NARRATIVE FRAGMENTS OF SATISFIED EASE (21/148, 14.2%)
Here are some examples:
- We are a team, and there should be no me/you but we. Collection
- They’re doing the best they can. Luckily, everyone is busy.
- We’ve created a whole group, they’re competent and willing, they support each other.
- They must be happy to work with me! In the sense that by estimating and recognizing the human and technical capabilities of its manager, one can work towards a single objective. I feel respect and affection from my colleagues
- They’re interesting, cultured people who want to grow up.
- They share my values and this is crucial for the work climate because it allows us to support each other and aim for challenging goals
- They’re my second family. They do not have the same aptitudes as me, but there is a deep mutual respect and a desire to share and grow together.
NARRATIVE FRAGMENTS OF PARTIAL EASE (16/148, 10.8%)
Here are some examples:
- On average they are quite aligned in design and identification of criticalities
- They help me not to succumb, to face complexity with a smile of awareness
- For the most part, they’re collaborative and constructive.
AMBIVALENT NARRATIVE FRAGMENTS (42/148, 28.4%)
Here are some examples:
- Some have no awareness and sense of belonging, others think they are “doing it alone”, others have vision and capacity for networking and sharing
- Usually they are resources and I usually see them committed, responsible and available The bad times are often due to unfulfilled expectations (including economic ones), or lack of coordination, isolation and not involvement
- I work with a nursing team. That I see tired, demotivated. They do their best and they’re great. But they’re systematically decimated and replaced with people who don’t have the aptitude and communication skills.
- Most of the co-workers and coworkers are valid. Someone is hiding behind false physical limitations and is little involved in the fair division of the workload. Relations are good with everyone except for rare exceptions. They are good people and good professionals.
- There is a good 65% of colleagues in the department with whom there is a very good collaboration. Outside of the anesthesia and resuscitation service, collaboration becomes increasingly difficult.
NARRATIVE FRAGMENTS OF PARTIAL DISCOMFORT (35/148, 23.6%)
Here are some examples:
- They don’t have my same dedication
- They feel overwhelmed, disappointed, including bullied like me! In spite of everything we remain but who can leave, leave this health institution that takes on the aspect of totalitarianism. We must be willing to fight for the sick and for ourselves as professionals
- At the moment I see so many demotivated people, in the last year 3 wellprepared colleagues have resigned to work in Switzerland.
- Unfortunately, the majority is as disillusioned as I am
NARRATIVE FRAGMENTS OF TOTAL DISCOMFORT (34/148, 23%)
Here are some examples:
I feel like I have to drag them over.
- Often they work passively
- Demotivated
- They’re listless, demotivated, shallow
- Not interested in the group, very selfreferential , no appetite for change
- Many are disillusioned, tired, angry. It is difficult to carry out projects, many stop at routine without wondering if the same is useful to patients. Demonstration also has negative repercussions in interpersonal relationships, the climate in the working group is increasingly cold and aseptic, the other is often seen as a danger, certainly not a friendly face.
- They’re like dead
- ….if they can leave (retiring, private, firing, etc.) Who remains – of the doctors with more seniority and work experience – is because they need to work The younger doctors just hired limit the professional commitments so as to strictly adhere to the hours of work provided by the contract trying to avoid the surplus of hours and of untaken (and not monetised) leave as happened instead to the older doctors
- They are not all up to the job today and are demotivated
Below is a graph of the total of 174 respondents to the survey 148 who testified in this specific section (about 85% of the total).
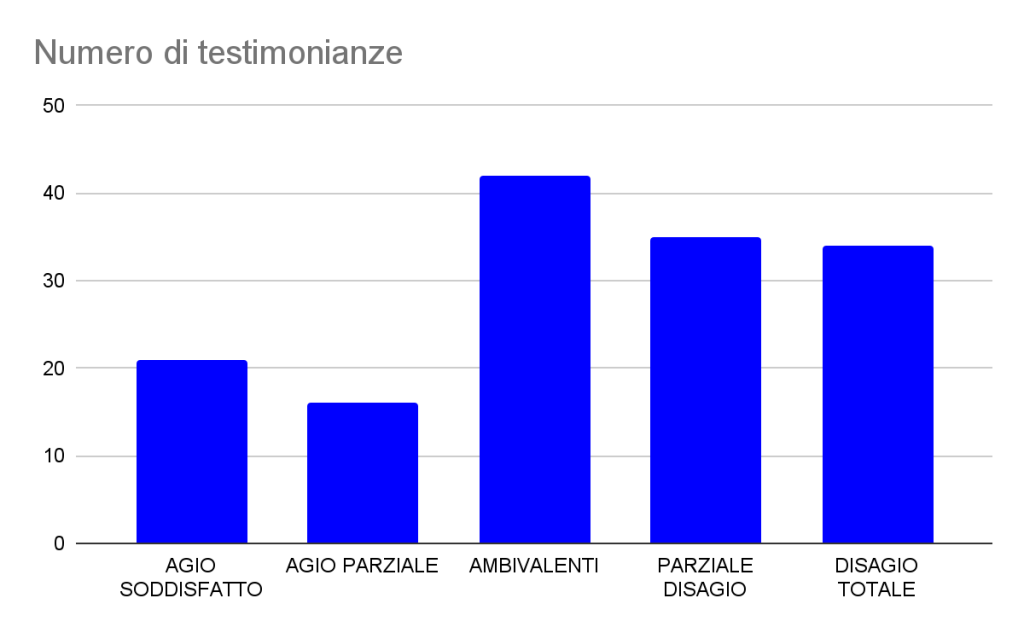
Figure 4: Types of responses to the narrative stimulus “The others working with me…” and numerical frequency (N=148)
In the discussion about colleagues, a new scenario opens that blurs the outlined lines, putting a better balance between the different sections. Generally speaking, there are signs of deep respect for colleagues and staff, a sign of a working climate characterized by a sense of solidarity. However, one cannot overlook the fact that sometimes employees seem to share the same experiences of discomfort and alienation in the workplace. This may suggest that, although mutual consideration is present, there is still a layer of widespread dissatisfaction involving the whole group.
Interestingly, the survey also highlights criticism of colleagues themselves, giving voice to a perception that they may be an integral part of the problem. This observation opens a reflection on internal dynamics within the working group that could contribute to the general malaise. Perhaps, in some cases, the lack of effective communication or optimal collaboration between colleagues can become a source of frustration or dissent.
Ultimately, the complexity of coworker relationships requires a deeper view and a complete understanding of the workplace. The survey suggests that while mutual respect is predominant, there are still internal dynamics that merit special attention. Opening up to dialog and strengthening the relationship between colleagues could be an important key to improving the overall working environment.
NARRATIVE STIMULUS PEOPLE I CARE ABOUT…
Figure 5 Word Cloud of the replies to the narrative stimulus “The people I cure…”
In this section of our anonymous and voluntary narrative survey we asked doctors, nurses and health care professionals how they feel about working in their organization. What you find listed below are some narrative fragments that we have selected for you from all that have been sent to us.
In the cloud of words stand out the words “gratitude”, “grateful” and “satisfied”, “good” “always”, “often” as it is normal that it is reading the testimonies. Much smaller is the presence of “difficulties”, “fragile” and “problems”.
THE PEOPLE I TREAT…NARRATIVE FRAGMENTS OF SATISFIED EASE (51/146, 34.9%)
Here are some examples:
- I owe my gratitude to them because patients are always teachers.
- Each of them is a unique, fragile and wonderful world from which I receive the dimension of the importance, sadness and beauty of life
- I’m taking preliminary care of surgery. “I feel” I’m happy with my interview. I often hear you say: why has no doctor ever spoken to us like you today? They’re sorry when I say I won’t be in the room with them. I think I’m doing a good job, despite everything.
- they have very different histories; my mode of care is expressed above all in the form of listening, not being a health figure. I feel their gratitude.
- I am happy with the service i offer and am grateful
- They recognize that “time devoted is time of healing,” sharing, confrontation, a word, standing next to it. And this is true not only for them, but also for me, because it is this motivation and recognition that keeps going, but more and more is failing
- They’re beautiful
- They are happy to be accompanied, if they feel well guided they are very cooperative
- They’re fantastic! They are great heroes and heroes who in their daily lives manage to field enormous psychophysical resources to fight their own disease and make sense of every new day despite the difficulties and often a severe and difficult loneliness
- I’m my end
- They all have esteem and affection towards meI’m happy and they keep saying luckily we are there, you are angels
- I’m in the middle. I listen to their story and I find a way to get into a posture that allows me to sartorially relate in order to get a 360 degree treatment path
- I am my satisfaction. They’re stares. They are graces expressed even with small gestures or tears. Or nothing, I realize it’s okay.
NARRATIVE FRAGMENTS OF PARTIAL EASE (23/146, 15.7%)
Here are some examples:
- They generally understand our problems, thank us. But there are difficult times ahead, they must be managed.
- They see that despite the difficulties we try to satisfy their physical and psychological needs as best as possible
AMBIVALENT NARRATIVE FRAGMENTS (33/146, 22.6%)
Here are some examples:
- They’re hard to cure, but if you can hook them up and get on with them, they’re great. Unfortunately it is not always so, there is also frustration
- Some seek help, others exploit me for benefits
- They are in great difficulty, not only because of the diseases they suffer (they, but also their families), but also because of the organizational incapacity of the departments and the bureaucracy they are victims of, as well as the lack of facilities or domestic support services. They almost always have a lot of gratitude towards us, which is what keeps you going.
- They experience situations of stress and trauma and struggle to cope with the situation they face and adapt to. Attitudes of anxiety, rejection are common and being close to people allowing to express even negative emotions is a daily task. Many express gratitude for what we do and this allows me to reinforce my motivation to do what I do, especially when I feel fatigue.
- Despite all the problems of systematic shortage of staff and serious cases, I work in a complex department of cancer surgery and hepatopathic gastroenterology with many beds, I think our patients are satisfied with our care. Some of us are aware of our difficulties, show understanding and gratitude. Others unfortunately do not.
NARRATIVE FRAGMENTS OF PARTIAL DISCOMFORT (30/146, 20.5%)
Here are some examples:
- Often even patients seem to want only easy answers, as if they were products of a supermarket.
- They are fragile people who are not adequately supported due to lack of time on the part of professional staff
- They would like more from me I am powerless and burdened with other bureaucratic obligations etc etc etc etc
- they think it’s all our fault. Many are angry about everything we cannot do or offer, without stopping to recognize what we give. Not everyone, of course
- The nursing grounds on which people go to work have changed a lot over the years. Increase in large elderly and/or multimorbidity patients. High expectations on the part of users often not adapted to the state of affairs. A general sense and preconception of distrust of the users towards the doctor. Increased level of rudeness and aggression. Then there are pleasant patients with whom a great relationship is established, but they are a minority. It often happens that among us healthcare professionals we wonder pleasantly in front of a kind and polite user, when instead the collaboration doctor/patient, nurse/patient should be the norm.
NARRATIVE FRAGMENTS OF TOTAL DISCOMFORT (9/146, 6.2%)
Here are some examples:
- They are increasingly fragile and destabilized, placed in care settings that make pathways often based on reducing the time spent on treatment difficult. They complain of poor communication with the doctors, of a sense of abandonment that undermines a healthy relationship aimed at treatment.
- They are most ungrateful and pretentious
- They are often scarce for education, often rude or aggressive
Below is a graph of the total of 174 participants in the survey 146 left their testimony in this specific section (about 83.9% of the total)
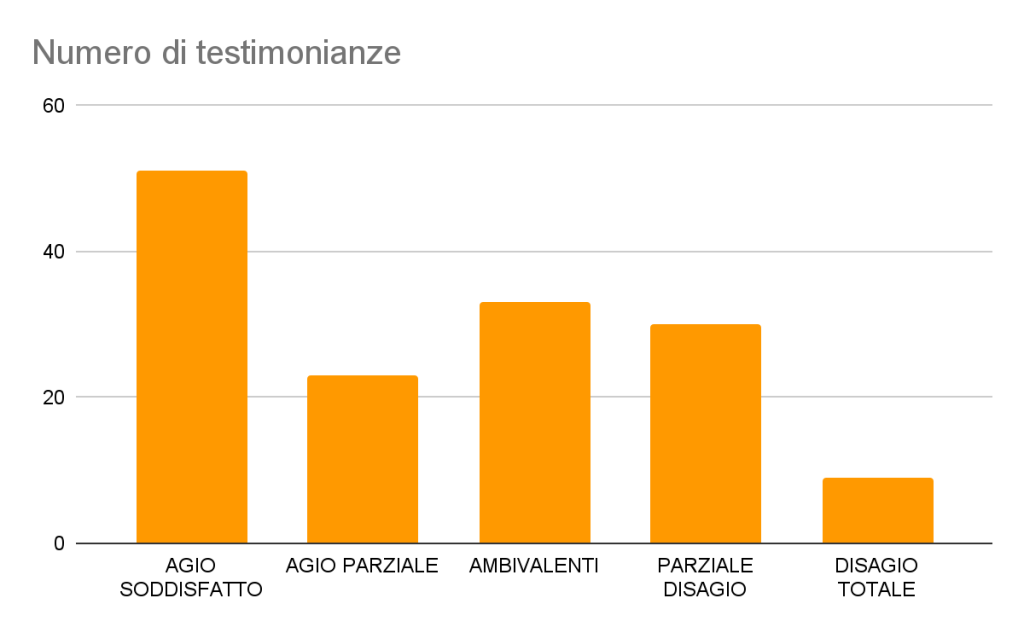
Figure 5: Types of responses to the narrative stimulus “The People I Cure…” and numerical frequency (N=146)
This section is a departure from the others we have discussed so far. Significantly, the category that prevails in this case is that relating to the comfort satisfied. The results obtained are consistent with those obtained from the Maslach test: patients are often perceived by healthcare professionals as the only positive element of their activity. Love for the care of the other is often the only motivation that drives them to persevere in this profession, characterized by an increasing management complexity.
The gratitude expressed by patients is shown to be of non-minor importance to the overall satisfaction of doctors and nurses. The number of people reporting total discomfort is extremely limited, which is also important in this context. This provides a significant cross-section of the healthcare workplace, highlighting how the relationship with patients and the sense of gratification that comes with their well-being can be key motivations for healthcare professionals.
It is interesting to note that, despite the ever-increasing challenges and complexities related to the management of work in the health sector, the love for the care of others emerges as a driving force capable of countering the difficulties encountered daily. Ultimately, this study highlights the centrality of human relations and gratitude in the field of professional satisfaction in the medical context.
CONCLUSIONS
Which policies?
Let’s broaden the subject and consider the issue of the medic’s retirement* at 72: it is a strategy due to the lack of health programming that has existed since the big cuts in health care, the excessive closed numbers to the medical faculty – (news of 23 January 2024, probably the Swiss and French model will come into force, so there will no longer be closed numbers, but the value of students will be measured after the first exams to be passed) from contracts unattractive for doctors and almost “insulting” for nurses. Perhaps the politicians who promoted retirement at 72 are unaware of the fatigue of night guards, strained nerves in intensive care, or the constant contact with death in palliative care services.
Curating is a wonderful profession (and we understand it from how “happy” the care professionals are with their patients) but there is also a time necessary for self-care: splendid curators over seventy years who have responded to us, yet they are people who have “chosen” on a voluntary basis to continue to treat, they have not remained by obligation. The truth is that “the King if not naked is underdressed” in terms of system and resources. Now health professions need to be made looser, university courses need to be less obsolete (full of notionism) and richer in the education derived from humanities. And expand to the young, go and collect them on the open days of high school, sending those doctors* and nurses* as witnesses who still believe in the mission to speak to them and explain the beauty of the act of care.
Combine the care professions with biology, natural and social sciences, philosophy, the arts from university, (STEM disciplines with SHAPE disciplines) and all the time of the profession, so that it is a Life Long Learning that goes to fill the vessels half empty energetically.
But let us not talk about professionals* cold and detached health professionals*: here, in the middle of this cold winter, there is warmth with the patients, and so much feeling of Common Good to save and protect: the request, as also read from the narrative part, is that of having recognition. It is time for the summit to take care to thank and say that its staff members are worth it, to recognize and rebuild the interdependence of teams, to find the economic resources to pay them adequately, and to motivate them through the possibility of people taking time for themselves, to rest without sucking them “in the waves of the tsunamis”.

Figure 6: Kanagawa’s Great Wave, Hokusai
They thank all the professionals who have left their voices behind and shared the project, believing in this research, which many of them have appreciated as necessary. We thank Dr. Delia Duccoli for her careful supervision.

