 Come, come, you froward and unable worms!
Come, come, you froward and unable worms!
My mind hath been as big as one of yours,
My heart as great, my reason haply more,
To bandy word for word and frown for frown;
But now I see our lances are but straws,
Our strength as weak, our weakness past compare,
That seeming to be most which we indeed least are.
The taming of the Shrew, William Shakespeare
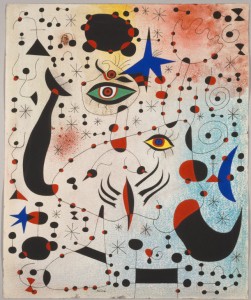
In the last verses of the Taming of the Shrew Shakespeare puts into Catharina mouth words of an infinite tenderness, that tenderness which will be the keys for her marrieg of love with Petrucho. Through the whole comedy she has been a master using the dialectic features, and she has been always winning all her possible competitors using her sharp mind. To conquer her love, the “in love” Petrucho acts as crazy, outside from every standard rule and from routine protocols, but never using brutal force towards her. And Shakespeare’s text, suggests that successful men and women work in tandem rather than in hierarchal fashion, and so doing elevates not only the husband and the wife, but by extension, everyone and everything they come into contact with, as well.
When thinking to the last two decades, the Evidence-Based Medicine (EBM) has become the golden marriage for science and caring; no cure which was not proved to be effective in comparison to a certain golden standard should have been considered worth for a medical consideration. The definition of EBM provided by David Sackett in 1996 is “the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients”. Almost twenty years have passed, and the EBM colonized North America, European countries, moving with a globalization approach to be acknowledged by the World Health Organization as the primum movens of the evolution of clinical science. It was and it has been definitely a tool to take out medical science from a paternalistic and superhuman approach displayed by the physicians: it has been at that time, historically, when arose a very relevant value to counteract the power of physicians above patients, the dilemma quite impossible to solve of the asymmetry in the patients- physicians relationship. Reading the definition of Sackett we are faced to solve a huge issue: individual patients. Individual is a singularity, patients are in a plural definition.
This shade of this definition has been quite neglected by the clinical trial makers, for whom only populations and subgroups of patients had been important: the individuality does not count. Sackett in his words was already anticipating a philosophical paradox: how individual solution can fit for populations? He was introducing a caveat in its own – and his own school – discipline. Despite to this careful formulation of his thought EBM developed untamed, and become a giant in scientific communities, medical congresses and hospital management: only evidence based therapeutic solutions are reimbursed, especially in these years of shrinkage of resources.
“It is time to stop overloading doctors with evidence and deploying fast-talking industry salespeople to manipulate them with clever marketing pitches. …. Research-derived facts about the average patient must not outweigh individual patients’ observations of their own bodies and illnesses. New processes for capturing and accommodating patients ’personal experiences’ – which are typically idiosyncratic, subjective, and impossible to standardize – would go a long way toward ensuring that each patient receives the right treatment. The medical community must develop the science of shared decision-making, in which epidemiological evidence informs conversations about what matters to the patient and how best to achieve those goals. In doing so, we can take evidence-based medicine beyond its current limits and develop a holistic approach that accounts for patients’ experience of illness and promotes good clinical practice”.
Is Evidence Based Medicine broken is a title of this post by the epidemiologist and narratologist Greenhalgh, published in October 2014; her considerations move from a survey with UK doctors run through the British Medical Journal in 2014, asking to its its readers whether evidence-based medicine was malfunctioning. The responses were almost evenly split: 51% answered positively, and 49% negatively. There is impossibility of finding a consensus facing this data; a slight democracy in favour of an EBM could be sensed, but a part from this sensation, the logic of scientific methodology is seriously put in danger. Main causes reported in this article are the choice of a golden standard in trials which excluded other alternatives not acknowledged valid by scientific community but, on the contrary, deemed useful by the medical praxis, as yoga for instance, the invention of ghost diseases by different stakeholders – academics and private companies as “female sexual arousal disorder” or, in the implementation of EBM , the decision support tools unable to handle and master inability the messy, unpredictable, real-world clinical practice.
To these considerations, we could add some other biases and poor outcomes of EBM: the exclusion of patients with comorbidities, very likely old patients, bias already detected at the down of EBM in 1995 in a challenging article published in middle 90s, which was already arguing whether the scientific totem of the new millennium could have been Evidence Based or Evidence Biased Medicine. Another bias is due to the statistical huge sample size which are able to demonstrate only statistically significant results that from a clinical meaningful view count less than a pinpoint “The larger the effect of a specific treatment, the smaller the required trial”.
Publication bias is another pitfall which has remarked for EBM; for instance, for antidepressant therapy the FDA deemed 38 of 74 submitted studies (51%) positive, and all but 1 of the 38 were published on scientific journals. Other 36 studies (49%) were deemed by the FDA to be either negative (24 studies) or questionable (12). Of these 36 studies, 3 were published as not positive, whereas the remaining 33 either were not published (22 studies) or were published, as Turner states, positive (11) and therefore conflicted with the FDA’s conclusion. Overall, the studies that the FDA judged as positive were approximately 12 times as likely to be published in a way that agreed with the FDA analysis as were studies with nonpositive results according to the FDA (risk ratio, 11.7; 95% confidence interval [CI], 6.2 to 22.0; P<0.001). Here statistics matter and show in a very likely way that the publication bias exists despite there is a scientific rule which ask to publish all results, the good and the poor ones.
Even the Economist starts to interest itself to science, mainly because of reliability of pharmaceutical and life sciences drugs and devices portfolios, and related academics habits and states in middle October 2013: “The obligation to “publish or perish” has come to rule over academic life. Competition for jobs is cut-throat. ….Careerism also encourages exaggeration and the cherry-picking of results. In order to safeguard their exclusivity, the leading journals impose high rejection rates: in excess of 90% of submitted manuscripts. The most striking findings have the greatest chance of making it onto the page. Little wonder that one in three researchers knows of a colleague who has pepped up a paper by, say, excluding inconvenient data from results “based on a gut feeling”. And as more research teams around the world work on a problem, the odds shorten that at least one will fall prey to an honest confusion between the sweet signal of a genuine discovery and a freak of the statistical noise. Such spurious correlations are often recorded in journals eager for startling papers.” The statistical noise is also here coming to cover the genuine discovery, which cannot allow itself big trials to be tested, or it is so innovative that it is neglected by the caste of the scientific academy. Numbers are self explanatory. “A rule of thumb among biotechnology venture-capitalists is that half of published research cannot be replicated. Even that may be optimistic. Last year researchers at one biotech firm, Amgen, found they could reproduce just six of 53 “landmark” studies in cancer research. Earlier, a group at Bayer, a drug company, managed to repeat just a quarter of 67 similarly important papers. A leading computer scientist frets that three-quarters of papers in his subfield are bunk. In 2000-10 roughly 80,000 patients took part in clinical trials based on research that was later retracted because of mistakes or improprieties.” The Economist is very tough, criticize and talks about careerism and possible fraud: but putting together the complexity of the human being of the patients as already described by Greenhalgh and these information we could come up that there is something beyond the number of publications, the bias of EBM, the careerism, the earnings of the Health care system and life sciences: there is the impossibility or huge difficulty to transfer the real genuine science from center to center, from paper to paper, for some hypothetical reasons that I wish to list: first, every text in in a unique context and so only, maybe, in a perfect physics close system the experiment can reproduce itself. Second, the way in which scientific publications are structured is so structured that obstructs the possibility to transfer the intangible knowledge, the shades according which the specific scientific test can be repeated. It will never be the same. Nothing can ever happen twice as Wislawa Szymborsk,, awarded in 1996 with the Nobel in literature, writes:
Nothing twice.
Nothing can ever happen twice.
In consequence, the sorry fact is
that we arrive here improvised
and leave without the chance to practice.
Even if there is no one dumber,
if you’re the planet’s biggest dunce,
you can’t repeat the class in summer:
this course is only offered once….
And perhaps nothing happens exactly in the same way also in the world of science: and this is why is so difficult to repeat in the same manner the scientific experiment which was carried out first at Karolinska Institute and then in a less sounded scientific research center: scientific journals and scientific congress as for they are nowadays, publications are so rigid, so strict, so armoured that in the last years they seem a poor vehicle to transfer knowledge, that knowledge which is fresh, not protected by strengthened economic interest, still fragile, and not so easy classifiable with a “yes” or “no” answer.
I have been already and yet constantly facing myself with the orthodoxy of peer reviewer for EBM journal: after having submitted Narrative Medicine to highlight values of Italian pain therapists in a changing healthcare system, a narrative paper, to the European reference Journal of the pain treatment, I received the very first time this fast reply by the editor in chief: “We will not forward your article to any referees, because we publish only quantitative results”. Here the totems are numbers, digits, probabilities: no text, no context in allowed. Good news is that we have been able to publish our work with another editor. But what amazed me, although I must admit I was quite angry for the answer, was the superficiality with which our paper was considered. EBM holds the keys of current scientific paradies in the behaviours of most reviewers of scientific papers which are the fruit of scientific research. And this is an orthodoxy, we could define it also an abuse of power, which has to be tamed: not only numbers from trials, but also numbers from real life world. And beyond these not only digits, but also narratives which show the complexity and the subjectivity of the world of providers of care and patients and their caregivers.
Greenhalgh writes: “Indeed, only Aunt Nora can tell you how her celiac disease behaves. She also happens to be opposed to taking blue-colored pills. And she insists that, years ago, when she took drug x, it made her feel like a new woman – despite the fact that, in 1,000 patients, drug x has demonstrated, on average, no effect. The computer model’s treatment recommendations would probably not work for Aunt Nora”.
EBM could have become the superb Catharina in the Taming of the Shrew, which is softned by the narrative and bizarre and odds manners of Petrucho, the antilogic character which falls in love for her: But now I see our lances are but straws. The EBM shrew should see that lances are just straws and only if it loses its arrogance and includes the poetry of humanitas of caring could transform herself in a beautiful woman in love for the very first time and win a happy ending. Without any hierarchy, just the win win situation of logic and intuitivity and emotions.
